20 July 2015
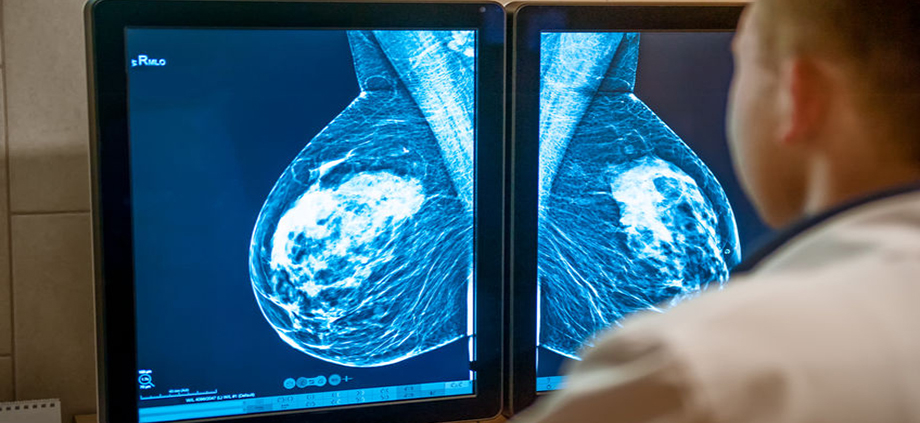
This is not a new question, and I promise there will be many parts to this story. The latest: Breast Cancer Screening, Incidence and Mortality Across US Counties, published in the July 2015 issue of JAMA Internal Medicine. The authors of the study noted that rates of early breast cancer detection have increased with the widespread use of screening mammography, but death rates from breast cancer have not decreased, leading to the conclusion that many breast cancers are “overdiagnosed”.
One would expect that if there were an increase in the number of early breast cancers detected due to screening mammography, fewer women would subsequently die from breast cancer. Isn’t early detection the key to survival? A reasonable question that is raised from this study is “What is the value of screening mammography?”. First, several points:
- The authors noted that the rates of early breast cancer, especially DCIS, have increased significantly with the widespread use of screening mammography.
- It is well known that some breast cancers have such an indolent biologic behavior that they will never become a threat to a breast or to a life.
- The more we screen, the more we find. Not everything needs to be found.
- Finding indolent lesions is considered “overdiagnosis”. Treating these lesions with traditional surgery, radiation and other treatments is considered “overtreatment”.
- Early detection does not always equal cure. Some breast cancers have a very aggressive behavior, and may prove to be fatal even when diagnosed in early stages.
Before you cancel your upcoming mammogram, appointment, some limitations of the study were pointed out in an accompanying editorial: Effect of Screening Mammography on Cancer Incidence and Mortality. One of the biggest criticisms is how the study was actually conducted, using the “ecological method”, which studies large groups, not individuals. It is not possible to tell if the women who were diagnosed with breast cancer are the same ones that subsequently died due to the disease. Other limitations of this of study are that no information is available on tumor subtypes or adjuvant therapy (chemotherapy, hormonal therapy and radiation). Another limitation of the study is that it evaluated data over a 10 year period, which might not be long enough to have an impact on survival rates. Finally, it was discussed that there was the potential for “confounding bias” – factors associated with an increased risk of breast cancer might also be associated with an increased rate of obtaining screening mammograms. [For a good discussion of the types of bias that may be present in research studies, review this article from HealthKnowledge.]
There is no question that we are finding more early stage breast cancers, including DCIS. There is much debate on whether or not DCIS even represents “cancer”. But the reality is that while we recognize that not all cancers will progress, we do not yet have the ability to predict the behavior of a cancer with certainty for an individual woman. We do not yet have that crystal ball.
So now what? The conclusion always seems to be “ask your doctor”. But physicians do not have all of the answers. What is clear is that the decision to begin or continue screening mammography is no longer automatic – discussion about the benefits of mammography, the potential harms, a woman’s own risk tolerance, and personal beliefs is necessary – this is the essence of shared decision making.
Various online tools have been developed to help women make more informed decisions. One is Weill Cornell Medical College’s Breast Screening Decisions, meant to be used by women in their 40’s. This is a start. We also need to develop that “cancer crystal ball”, which will allow us to more accurately predict who will develop cancer, and the behavior of a cancer that has developed. We’re just not there yet. Stay tuned as this is certainly not the last word on this issue.






Trackbacks & Pingbacks
[…] Dr Deanna Attai weighs in on the mammography debate. […]
Comments are closed.