3 May 2019
The American Society of Breast Surgeons (ASBrS) has updated their screening mammography guideline, recommending that women of average risk begin annual screening mammograms at age 40. This update brings the ASBrS guideline more in line with those of the American College of Radiology and the Society of Breast Imaging, and are a departure from their previous guideline, which called for screening to start at age 45. The American Cancer Society recommends annual screening from age 45-54, followed by biennial screening with the opportunity for annual screening. The US Preventative Services Task Force recommends biennial screening starting at age 50.
The updated ASBrS guidelines recommend as a first step that all women undergo a formal risk assessment starting at age 25. Risk assessment involves using any one of a number of models to estimate 5-year and lifetime risk of breast cancer development. These models take into account age, family history, menstrual and pregnancy history as well as history of prior biopsy and racial / ethnic background. Some models take into account body mass index and breast density. The ASBrS guideline has additional recommendations, outlined below, depending on risk level. The recommendations listed for women at high risk of breast cancer are consistent with those of the American Cancer Society and National Comprehensive Cancer Network.

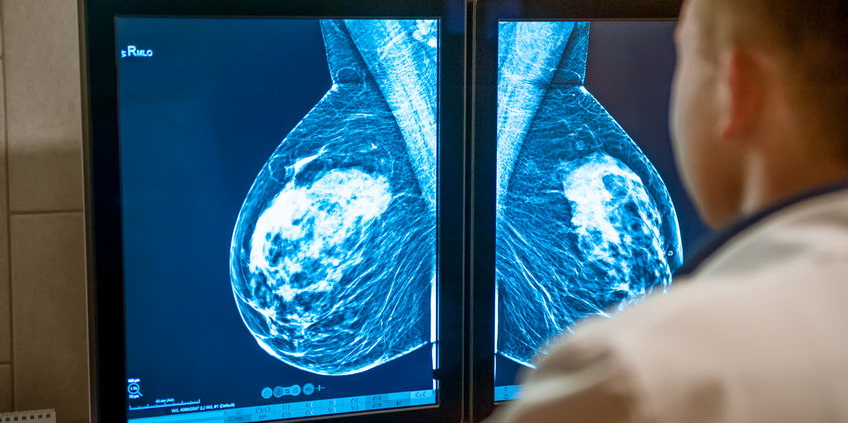
When to start and how often to perform screening mammography has been the subject of much debate over the years. The primary issue is the number of lives saved balanced against the harms of screening mammography. Harms include false negatives (cancer is not detected by the mammogram), false positives (suspicious areas that turn out to be benign) and recommendations for additional imaging (added cost and concerns about the potential effects of cumulative radiation). There have also been concerns raised about over-diagnosis and over-treatment: finding cancers that would never pose a threat to a woman’s health or life – but the patient is exposed to the potential harms of cancer therapy.
The goal of screening is not to detect all cancers – otherwise we would recommend complete body imaging for everyone. The goal of screening is to improve the survival from the cancers that are detected. An ideal screening test is relatively inexpensive and performs equally well in the patient population undergoing the screening. Mammography is acknowledged to be an imperfect screening tool – while relatively inexpensive and safe, it simply does not perform the same in women with breasts of different ages and densities. Approximately 1000 women need to be screened to detect 2 – 7 breast cancers, and mammography performs best in women age 50-74. In younger women, a few cancers will be detected, and there may be a survival benefit. However, because breast cancer is less common in younger women, a larger number of women need to be screened to find a single cancer, increasing the likelihood of a harm. The benefits of screening do not always outweigh the risks – at least for an individual patient.
It is also important to note that some of the new ASBrS recommendations, such as 3D mammography as the preferred type of mammogram, supplemental ultrasound in women with dense breasts, and MRI for all women with a history of breast cancer, are still undergoing investigation and are not always covered by insurance. We know that these studies will find additional cancers, but we do not yet have data on improved outcomes. My patients know that I am fond of saying “the more we look, the more we find, but not everything we find needs to be found.”
Two ongoing studies will hopefully provide additional information regarding 3D mammography and screening interval:
- The TMIST trial is a national multi-center study assessing the performance of 3D compared to 2D digital mammography. This study will assess rates of cancer detection, callbacks and benign biopsies as well as biology of the tumors detected and outcomes.
- The WISDOM study is evaluating a risk-based screening approach. After a comprehensive risk assessment, genetic testing, and assessment of risk tolerance, patients are assigned annual versus biennial screening. Women can self-enroll in this study (disclosure – I am not involved with the study team but I am enrolled in the study as a participant) and do not have to change mammography facility.
Until we are at a point when an individual woman’s level of risk can be accurately predicted, there is no definitive “best” screening guideline to follow. Recognizing the potential harms of screening mammography, it is no longer appropriate for physicians to simply hand out an order for an annual screening mammogram for all women starting at age 40. A balanced discussion, taking into account an individual woman’s risk and level of risk tolerance as well as the absolute potential benefits and harms of mammography is indicated. These discussions are nuanced and take time. Various genomic assays are being evaluated and it is hopeful that we will at some point have a test that can accurately predict a woman’s risk of breast cancer – which can then be used to provide more tailored guidance regarding imaging. Until that time (and I hate to end this way…), talk to your physician and medical team about what screening option is right for you.