8 May 2017
As a past-president of the American Society of Breast Surgeons I am probably more than a little biased. However, as always, the annual meeting held April 26-30th in Las Vegas was terrific. Topics including the full spectrum of breast disease, including benign and high risk lesions, genetic testing, breast cancer diagnosis and treatment including medical and radiation oncology updates, and metastatic disease.
The press briefing highlighted 3 abstracts which showed that:
- Modern therapy for inflammatory breast cancer is associated with better outcomes than historically seen
- Post-treatment lymphedema is related to a combination of treatments including surgery, radiation therapy, and chemotherapy – not just from surgery
- Patients with DCIS have a 5 year risk of developing a cancer in the other breast of 2.8% and a 10 year risk of 5.6%, and patients should be discouraged from undergoing bilateral mastectomy for this condition. Developing a new cancer in the previously treated breast was twice as likely as developing a new cancer in the opposite breast, and the use of tamoxifen reduced the likelihood of any recurrence.
Dr. Nathalie Johnson moderated a pre-meeting course on Building a Breast Cancer Survivorship Program. I was invited to speak on Traditional Versus Virtual – Options for Patient Support and Education. Just as it can be challenging to choose between cake and ice cream (2 really good things), patients note advantages to both in person and online support and education. It doesn’t have to be one or the other – do what works for YOU! My slides are posted on SlideShare.
During the general sessions, a few topics stood out to me:
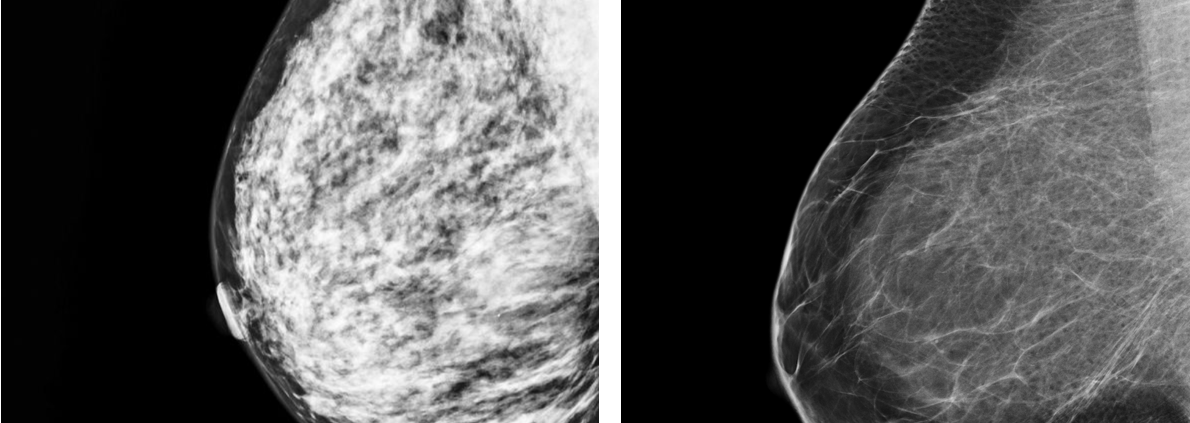
Dr. Shelley Hwang from Duke University spoke on DCIS subtyping and overtreatment. She noted that DCIS now comprises over 20% of all mammographically detected breast cancer. It is considered a “non-obligate precursor” of invasive cancer – the rate and likelihood of progression to invasive cancer are not clearly known. However, it is clear that some patients will never exhibit progression to invasive disease, and she discussed this in the context of thyroid and prostate cancer – two situations where we know that treatment in some patients will not provide the patient any benefit. The challenge is to sort out which patients will benefit from treatment and which ones will not. The COMET study is currently enrolling patients with low grade DCIS to in an attempt to help answer these questions.
Dr. Virginia Herrmann from Washington University in St. Louis spoke on non-genetic breast cancer risk factors. This is an important topic and I believe one that doesn’t get covered enough. She noted that hormone replacement therapy does increase risk – although the incremental risk is small and is seen only after about 5 years of use. However, longer term use does result in higher risk. Increased body mass index (BMI) is associated with risk – the risk of breast cancer is 30% higher in patients with a BMI greater than 31 kg/m2 compared to a BMI of 20 kg/m2. She noted that there is a linear relationship between alcohol intake and cancer risk, noting a 10% increase in risk for each 10 gm/day (for wine this is a little over 3 oz) increment in alcohol consumption. The risk is most associated with post-menopausal breast cancer, although in the study she quoted, only alcohol intake during age 50s was associated with an increased risk of postmenopausal breast cancer. She noted the association of ionizing radiation and breast cancer, and young women who received mantle (chest area) radiation for Hodgkin’s lymphoma have a markedly increased risk for developing breast cancer. She noted that breast cancer risk is increased in smokers, correlated with smoking intensity and duration. Finally, she noted the increased risk of breast cancer among soldiers stationed at Camp LeJune related to contaminated drinking water (tetrachloroethylene and trichloroethylene).
Dr. Tiffany Traina, a Memorial Sloan Kettering medical oncologist, gave a brief presentation about triple negative breast cancer: Searching For the Magic Bullet. There are several promising treatment strategies including targeting androgen receptors, the use of PARP-inhibitors in patients who have BRCA gene mutations, antibody-drug conjugates, immune modulating approaches, and targeted therapies based on tumor genomic profiles. Stay tuned – much more to come over the next few years related to this aggressive breast cancer subtype.
Dr. Lisa Newman, from the Henry Ford Health System in Detroit, spoke on Breast Cancer Outcomes: Disparities versus Biology. I have heard her speak on this topic multiple times over the years and always enjoy her excellent presentations. She noted that the incidence of breast cancer in black women is increasing, now close to that in white women. However, mortality rates for black women are higher than those for white women. There is an increased frequency of triple negative breast cancer in black women. She is involved in a research initiative evaluating the association between African ancestry and high risk breast cancer in white American women, African American women, and women in Ghana, including studying novel aspects of tumor biology and breast cancer stem cells – she is asking the question “are there differences in the oncogenic potential of mammary tissue that are associated with ancestry”? She concluded with what I felt was a powerful slide – 60% – 43% – 20%. Those were the survival rates for passengers on the Titanic who were in 1st – 2nd – 3rd class. She noted that healthcare outcomes are often dependent on access to care, and ended with a quote from Dr. Martin Luther King, Jr.: “Of all the forms of injustice, inequality in health care is the most shocking and inhumane”.
Dr. Stephen Edge, from the Roswell Park Cancer Institute, gave an update on the new American Joint Commission on Cancer staging system (AJCC 8th edition). Currently we stage breast cancer based on tumor size and lymph node status. However, it is recognized that that tumor biology plays an important role in prognosis and in some patients it may be more important that tumor size. The new staging system will incorporate tumor grade, Her2/neu status, ER/PR status, and Oncotype Dx status (if available) and should more accurately reflect prognosis. There are 422 lines in the new staging system – it will be impossible to memorize! Thankfully, he noted that the AJCC is working on a staging app.
The last day of the meeting held some great sessions, and the meeting room remained packed up until the very last minute. Dr. Ann Partridge from Dana Farber discussed special considerations in the young breast cancer patient. She noted that the disease is different, the patients are different, and the treatments should be different. Younger women have a higher likelihood to have more aggressive subtypes such as Her2/neu over-expressed and triple negative, and have lower survival rates than older women – even in those with the ER positive breast cancer. However, she cautioned not to over-treat patients based only on age. She noted that young age is not a contraindication for breast conservation, and that there is no clear improvement in mortality in patients who undergo more extensive surgery. She noted the need for improvements in treatment and support, including focused research and guidelines, which should lead to better outcomes.
Dr. Irene Wapnir from Stanford spoke on fertility preservation issues. She noted the various fertility options including medications and procedures. She also reviewed the POSITIVE trial, which will be assessing the risk of breast cancer relapse in patients who temporarily stop endocrine therapy to permit pregnancy, as well as to evaluate factors associated with successful pregnancy after interruption of endocrine therapy. She also stressed that fertility preservation should be discussed with any woman of childbearing age, whether or not she has had a prior pregnancy or a child – physicians won’t know what is important to their patients unless we ask!
Dr. Katherina Zabicki Calvillo from Dana Farber discussed breast cancer in pregnancy. She noted that 0.2-4.0% of breast cancers are diagnosed in pregnant patients – about 1 in 3000 pregnancies. She also noted that given the overall delay in childbearing (and the association of increasing age with breast cancer), the incidence of pregnancy-associated breast cancer will increase. Delays in diagnosis are related to hormonal changes which affect breast tissue making the exam more challenging, and that many patients and physicians assume that masses are related to pregnancy. She stressed that pregnancy termination is usually NOT required, but a multidisciplinary team approach is required. Many of these patients present in more advanced stages, but stage-for-stage, the prognosis is similar to non-pregnant patients with breast cancer. Chemotherapy can be given after the first trimester, but hormonal and Her2/neu targeted therapy should be avoided. She noted that mastectomy should be performed in the first and early 2nd trimester, and discussed the challenges of immediate reconstruction. Breast conservation could be considered in the late 2nd or 3rd trimester with post-lumpectomy radiation planned for after delivery.
Dr. Kevin Hughes from the Massachusetts General Hospital reviewed research studies that have found that in women over the age of 70 with early stage breast cancer, radiation therapy after lumpectomy may not be necessary. The CALGB 9343 study showed that survival rates were the same whether women received radiation therapy or not. Radiation therapy did reduce the likelihood of cancer returning in the breast (local recurrence) from about 4% in the untreated patients to about 1% in the treated patients (after 5 years of follow up). However it is important to realize that the majority of women in that study were treated with endocrine therapy, which can help reduce the risk of local recurrence. As with many decisions regarding breast cancer treatment, a careful discussion of the risks and benefits of each option is necessary.
Dr. Tina Hieken from the Mayo Clinic gave a very interesting talk on the microbiome and the impact on breast cancer. We normally co-exist with many bacteria – we have ten times the more microbial cells compared to human cells. These microbes carry out metabolic reactions that can be essential to human health. The genetic material (genome) of our microorganisms is called the microbiome. She and her colleagues studied breast tissue from women with and without breast cancer and found that the background breast microbiome is different in women with breast cancer compared to those with benign conditions. She concluded by noting that the future may involve using a microbial pattern to predict breast cancer risk, exploiting the microbiome to enhance treatment response, and that there may also be implications for a cancer prevention vaccine. The Washington Post recently covered her research – definitely worth a read for more information.
Dr. Anthony Lucci from MD Anderson discussed the “Ongoing Saga of Circulating Tumor Cells”. We would all like to see the day when a blood test can tell us with certainty if cancer has developed or returned – but we’re not there yet. After reviewing several studies evaluating both circulating tumor cells (CTC) and circulating “cell free” DNA, he concluded that this information does provide prognostic information in both metastatic and non-metastatic patients, but is not in the current ASCO or NCCN guidelines for guiding treatment. Combining the CTC status with response to preoperative chemotherapy may identify a low risk subset of patients, but noted that additional studies are needed before we can reach the ultimate goal which is improving outcomes by monitoring and responding to CTC and cell free DNA levels.
Dr. Manjeet Chadha from Mount Sinai spoke on repeat lumpectomy after prior lumpectomy and breast radiation. Traditionally, mastectomy has been recommended if cancer returns after lumpectomy and radiation therapy. On average, there is about a 10% risk of “in breast” recurrence after lumpectomy and radiation, but this will vary based on tumor and treatment type. She reviewed several studies evaluating the different types of focused or partial breast radiation that may be used in selected patients who experience recurrence of their breast cancer. She also called for additional studies in this area.
One of the last talks was by Dr. Mehra Golshan from Dana Farber. He spoke about the decision whether or not to operate on patients with breast cancer who present with Stage IV (metastatic) disease. Traditionally, we have not recommended surgery for patients with metastatic breast cancer as these patients were not expected to have long survival, and it was not felt that removal of the main tumor would impact survival. Evaluating existing studies has also been challenging because while some have shown a benefit to removal of the main tumor, the patients who underwent surgery in those studies tended to be younger and healthier. He concluded by noting that surgery in patients with Stage IV breast cancer is not standard of care, but some studies do support this practice. It is recommended that these patients be evaluated in a multidisciplinary forum and that treatment choices be individualized.
I returned from the meeting exhausted but energized. In addition to the scientific content, the meeting is an opportunity to connect with friends and colleagues across the country. I’m already looking forward to ASBrS 2018!
This post has not been endorsed by the American Society of Breast Surgeons.