7 February 2017
A research letter recently published in the Journal of the American Medical Association found that patients diagnosed with breast cancer were not appropriately referred for genetic counseling and testing.
The researchers used the SEER Registry to study the records of patients diagnosed between July 2013 – September 2014. Registry patients in the state of Georgia and Los Angeles County were mailed surveys which asked about their genetic counseling and testing experiences. Of the 2529 women who responded to the survey, 773 were considered to be high risk, in accordance with national guidelines. Of these high risk patients, only 39.6% reported having a genetic counseling session and only 52.9% had a genetic test. High risk patients reported lack of physician recommendation, not expense, as primary reason for not testing.
The authors noted that the lack of genetic testing in these patients was a missed opportunity to prevent ovarian and other cancer deaths among mutation carriers and their families. They concluded that the need for genetic testing may not be recognized by physicians, and they recommended that steps be taken to improve physician assessment of risk, assessment of patient desire for testing, and to optimize genetic counselor referral.
Limitations fo the study include that it was a retrospective (after the fact) survey. Patients may have received a recommendation for genetic testing but did not remember – this is often covered during the initial consultation which is a time of intense emotion. The study also only assessed patients from a limited geographic area – the state of Georgia and Los Angeles county. Despite these limitations, the study confirms others like it that demonstrate underutilization of genetic testing.
BRCA 1 and 2 genes are known as tumor suppressor genes, which code for proteins that repair DNA damage. When mutated, DNA damage cannot be repaired, and these patients are at high risk for developing breast, ovarian, and other cancers. Patients who have no signs of cancer may consider prophylactic surgery (made “famous” by Angelina Jolie). In these patients, prophylactic surgery can significantly reduce the risk of developing cancer. In patients who have already been diagnosed breast cancer and are found to carry a BRCA mutation, bilateral mastectomy is often recommended due to the high likelihood of developing another breast cancer, especially in BRCA 1 mutation carriers.
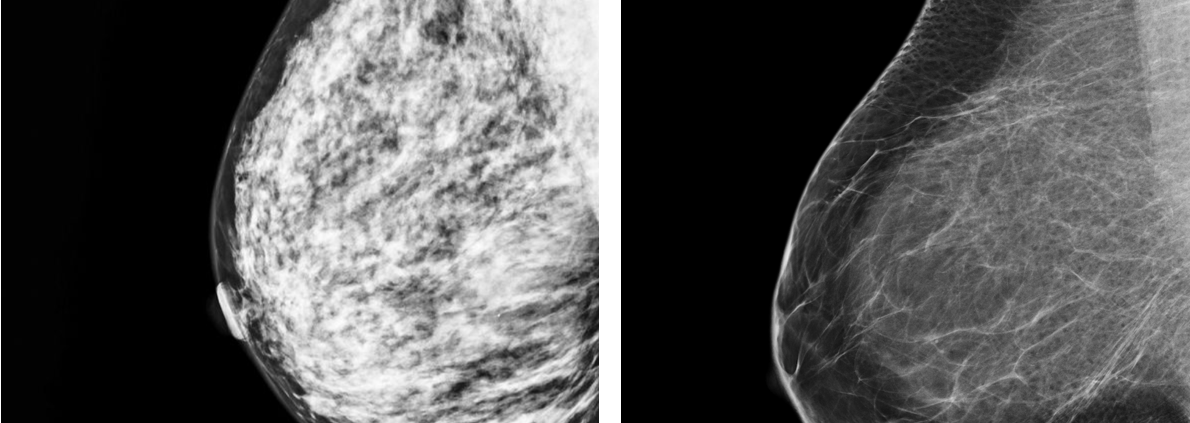
Guidelines for testing have changed over the years. If you were diagnosed with breast cancer several years ago, did not undergo testing, but currently meet one of the criteria for testing, discuss this with your physician. While you may not want to have any additional surgery, you may meet criteria for more intensive surveillance such as with MRI. In addition, test results coud have implications for other family members.
For more information:
FORCE – Facing our Risk of Cancer Empowered
National Cancer Institute – BRCA 1 and 2 Testing