The post Going Flat After Mastectomy appeared first on Dr Deanna Attai.
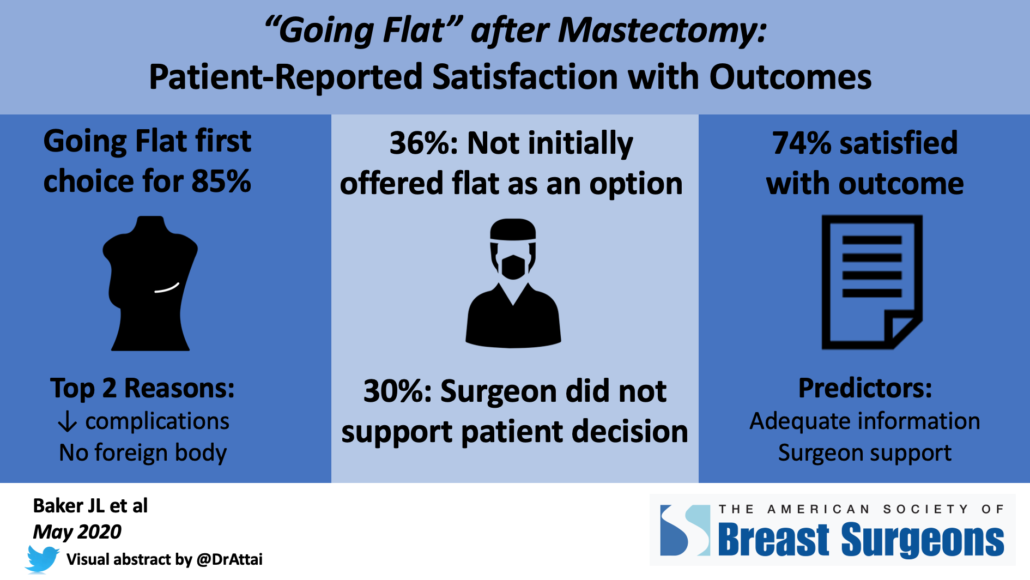
]]>Going Flat after mastectomy refers to not undergoing breast mound reconstruction after breast removal. Some patients are not candidates for reconstruction or it is not recommended, however many women may choose to “go flat” even when breast mound reconstruction is an option. This past October, we posted a research survey aimed at better understanding motivations to forgo reconstruction and to identify factors associated with postoperative satisfaction among patients who participate in online breast cancer communities.
The abstract and poster are now posted on the virtual meeting platform of the American Society of Breast Surgeons. Our findings include:
Demographics and timing of going flat:
- 940 women completed the survey, mean age was 53 (range 25 – 84)
- Most patients were white (94%), had private insurance (70%), and were from the US (74%) although 22 countries were represented
- 85% (801/940) did not undergo breast mound reconstruction at the time of mastectomy
- 15% (139/940) initially had reconstruction that was subsequently removed
Top 2 reasons for going flat:
- 72% desire to avoid foreign body such as an implant
- 71% perceived lower complication rate from the surgery
Communication:
- Only 64% were initially offered going flat as an option
- 30% felt that their surgeon did not support their decision to go flat
Satisfaction with outcome:
- 74% agreed or strongly agreed that they were satisfied with their surgical outcome
- Age, race, bra cup size, and history of prior breast mound reconstruction were not associated with postoperative satisfaction
- Strongest predictors of satisfaction were having adequate information about surgical options and surgeon support of the patient’s decision to go flat
Our findings reveal a need for additional research into factors that impact patient satisfaction as well as for surgeon education on how to optimally support women who are not interested in breast mound reconstruction.
It is important to note that any medical meeting abstract, whether an oral presentation or poster, has been evaluated by the meeting program committee but has not been subject to rigorous peer review as would occur with a formal manuscript submission. Abstracts (including ours) do not include the full set of results. It is not unusual for additional findings to be included in the eventual publication, some of which may be different than those presented in the abstract. However, we feel that these results are an important starting point for better understanding of patient motivations for going flat, and also point to a need for improved communication on the part of surgeons. We are in the process of completing a full analysis of the data and look forward to sharing the peer-reviewed publication when available.
On behalf of my co-authors, we would like to thank all who shared and participated in the survey!
The post Going Flat After Mastectomy appeared first on Dr Deanna Attai.
]]>The post Going Flat after Mastectomy – Research Survey appeared first on Dr Deanna Attai.
]]>Mastectomy (breast removal) rates continue to increase in the US. While reconstructive surgery is commonly performed after mastectomy, some patients opt to “go flat” or have no reconstruction. Some patients who have had reconstruction need to or choose to have the reconstruction reversed.
The aim of this study is to survey the “Going Flat” patient communities to assess patient satisfaction with their decision and results.
This survey is being conducted for research purposes. It is a UCLA research survey.
Patients should meet one of the following criteria to participate:
- Single or double mastectomy for any reason (including if lumpectomy was performed first) and decided not to have reconstruction (decided to “go flat”)
- Single or double mastectomy for any reason (including if lumpectomy was performed first), initially had reconstruction but then had reconstruction reversed or removed for any reason
This survey is voluntary and is completely anonymous. No identifying information, including internet protocol (IP) addresses, will be collected. There is no industry funding or sponsor for this survey. The survey should take approximately 15 minutes to complete. We value your time and your opinions. The anonymous data will be securely stored by the principal investigator and may be used for future research studies.
To participate in the survey, please click this link or cut and paste it into your web browser: https://uclahs.az1.qualtrics.com/jfe/form/SV_7UPj6wVtZev9UGx
For questions regarding this study, you may contact principal investigator Dr. Deanna Attai
- By phone: (818) 333-2555
- By email [email protected]
- By mail: 191 S. Buena Vista #415 Burbank, CA 91505
UCLA Office of the Human Research Protection Program (OHRPP):
If you have questions about your rights as a research subject, or if you have concerns or suggestions and you want to talk to someone other than the researchers, you may contact the UCLA OHRPP
- By phone: (310) 206-2040
- By email: [email protected]
- Or by mail: Box 951406, Los Angeles, CA 90095-1406
The post Going Flat after Mastectomy – Research Survey appeared first on Dr Deanna Attai.
]]>The post Patient Reported Outcomes and Complication Rates from Post-Mastectomy Reconstruction appeared first on Dr Deanna Attai.
]]>Two studies have recently been published which discuss patient reported outcomes and complication rates after post-mastectomy reconstruction surgery.
First a bit of background information on post-mastectomy reconstruction. The most commonly performed type of reconstruction utilizes implants. Often, a temporary tissue expander (TE) is placed by the plastic surgeon at the time of mastectomy. The TE is gradually “inflated” over time (using saline / salt water solution). When it gets to the desired size, a second operation is performed to exchange the TE for the implant. The TE and expansion process are necessary because after a mastectomy, the skin is thinned out (from removal of the breast tissue) and placement of the larger implant could compromise the blood supply to the skin and the healing process. However, a small percentage of patients are candidates for “direct to implant” reconstruction, which bypasses the TE step.
After mastectomy and implant reconstruction, patients usually spend 1-2 days in the hospital. The implants typically are placed below the pectoral (chest wall) muscle, which may result in pain and muscle spasm during the recovery period. A small percentage of patients may be candidates for “over the muscle” implant reconstruction. Implants may be filled with saline or silicone gel. Implants are foreign objects and are not meant to last forever – they may leak or may need to be replaced for other reasons. The FDA currently recommends that MRI be performed 3 years after silicone implant placement and then every other year to assess for “silent rupture” of silicone implants. However, insurance does not always cover these implant surveillance MRI scans. Potential complications of implant surgery include capsular contracture and infection which may require implant removal. Some women are bothered by the firm nature of some implants, or “rippling” which may be visible under the skin. Implants have recently been associated with a rare form of cancer – anaplastic large cell lymphoma. Routine mammogram, ultrasound or MRI are not generally recommended for breast cancer surveillance in patients who undergo mastectomy and implant reconstruction.
Autologous reconstruction (AR) utilizes the body’s own tissue. The TRAM (transverse rectus abdominus myocutaneous) flap was previously the most common type of AR. During the TRAM procedure, an incision is made in the lower portion of the abdomen (similar to a “tummy tuck” procedure) and the rectus muscle (responsible for “six-pack abs” in athletes) is removed with the overlying skin. That muscle and skin is then used to reconstruct the breast. The latissimus flap utilizes muscle and skin from the upper back. TRAM and latissimus flaps are generally performed as “pedicle” flaps – meaning their original blood supply stays intact.
With improvement in microvascular techniques, there has been an increase in the use of “free flaps” – this means that the original blood supply of the tissue for reconstruction is disconnected from its origin, and the blood vessels from the flap are sutured into blood vessels in the chest area. This has allowed the use of fat only for reconstruction, sparing the muscle. The most commonly utilized free flap is the DIEP (deep inferior epigastric perforator) flap. Other free flaps use fat from the thigh or buttock area.
AR surgeries are much longer – free flap procedures they may take up to 8-10 hours. Most patients are hospitalized for 4-5 days, including 1-2 days in the intensive care unit to monitor the blood supply to the flap. The recovery may be longer than implant reconstruction surgeries since healing needs to take place both in the chest area and in the abdomen (or thigh or buttock depending on the type of flap). The overall cosmetic result is generally more natural looking in patients undergoing AR. In patients having only one breast removed, it is much easier to “match” using AR techniques. The flap reconstruction also tends to feel much softer compared to implants (since it is the patient’s own fat) – but usually there is no sensation in the skin (or nipple if preserved) after mastectomy regardless of the type of reconstruction. The use of mammogram, ultrasound or MRI for surveillance in AR patients is controversial and practice varies considerably.
The 2 JAMA Surgery studies evaluated patient reported outcomes and complication rates after both implant and AR surgeries. The majority of patients were followed for 2 years. Overall, there were complications in 32.9% of patients – this includes everything from a minor skin infection treated with oral antibiotics to more serious complications including repeat surgery and reconstruction failure. 19.3% of patients required a repeat operation. 5.4% of patients had a failed reconstruction, where the implant or AR needed to be removed. At 2 years, patients undergoing AR had higher rates of complications including re-operations compared to patients who underwent implant reconstruction, although implant reconstruction procedures had higher rates of failure. Infections were also higher in implant reconstruction patients. In these studies, follow up only averaged 2 years – with longer follow up, patients with implant reconstruction may be found to have higher rates of complications since capsular contracture and implant leakage tend to develop over a longer period of time. Radiation during or after reconstruction, chemotherapy during or after reconstruction, and bilateral surgery were factors associated with higher complication rates in both groups of patients.
In evaluating patient reported outcomes, the authors noted that patients who underwent AR surgeries had higher rates of satisfaction with the reconstructed breast, physical well being of the chest, psychosocial well being, and sexual well being compared with those who underwent implant reconstruction. The AR patients did report lower measures of abdominal physical well being compared to implant reconstruction patients. Follow up in this study was also about 2 years for the majority of patients – only 21% of patients returned the survey at 3 years and 10.2% of participants returned the survey at 4 years. It is unclear if the implant reconstruction patients might report higher satisfaction levels if surveyed at a later point in time. The authors noted that due to the smaller number of patients who completed surveys at 3 and 4 years, conclusions in these groups of patients could be influenced by selection bias. Essentially that means that the small group may not be representative of the whole study population – for example, patients who are doing well might not be motivated to complete a lengthy survey compared to a patient who is having problems.
These findings should stress to patients that reconstruction is a “process not a procedure” – these are major operations with the potential for short and long term complications. I think that these 2 studies will contribute to how we discuss surgical options and potential complications with our patients, but the results may not make the decision-making process easier for patients. Patients trying to make a decision about surgery have already been told they have cancer – that alone is enough to shake even the strongest of clear thinkers. I have not figured out how to ensure that a patient is making a truly informed decision in this situation except through repeated discussion and questioning. As physicians we have made progress in helping our patients make decisions based on education and not fear. But is a truly informed decision even possible when the overriding reason for the decision is a potentially life threatening condition? I’m not so sure.
New York Times – One in Three Women Undergoing Breast Reconstruction Have Complications
The post Patient Reported Outcomes and Complication Rates from Post-Mastectomy Reconstruction appeared first on Dr Deanna Attai.
]]>The post Preoperative Breast MRI appeared first on Dr Deanna Attai.
]]>It is not uncommon that after a breast cancer diagnosis, a breast MRI is recommended. We know that there are limitations to mammography – it might not show everything of concern, especially in women with dense breast tissue. The idea behind preoperative MRI is that if there are other lesions, better to know about them and determine if they are cancerous or not, before going to surgery. This should lead to better surgical outcomes. Makes sense.
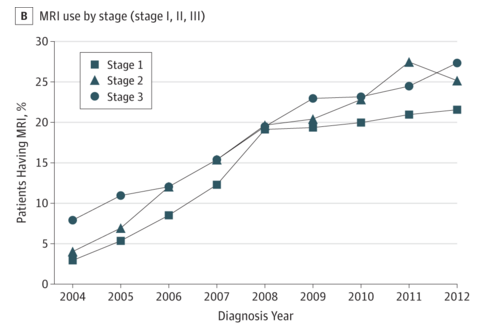
The problem is, studies have not been able to show a benefit to preoperative MRI. This was addressed in a recent issue of JAMA Oncology. Dr. Angel Arnaout and colleagues reported on the Use of Preoperative Magnetic Resonance Imaging for Breast Cancer: A Canadian Population-Based Study. In this retrospective population-based study, 53,015 patients with operable (early-stage) breast cancer were identified between 2003-2012.
Overall, close to 15% of patients underwent an MRI, and the use increased from 3% to 24% during the 10 year period.
Patients undergoing a preoperative MRI were more likely to be younger, of higher socioeconomic status, cared for in teaching hospitals, being cared for surgeons with a high volume of breast cancer cases, and cared for by younger surgeons. Preoperative MRI was associated with a higher likelihood of additional imaging and biopsies, greater than 30 day wait time to surgery, and higher rates of mastectomy as well as contralateral prophylactic mastectomy.
These findings were discussed by Drs. Habib Rahbar and Constance Lehman in an accompanying editorial. They pointed out several limitations in the study, such as not knowing the MRI results, and not having the genetic mutations status (such as BRCA 1/2) of the patients. However, they noted that “this study adds to the growing body of evidence that the use of MRI in the preoperative setting is associated with more aggressive surgery of the affected breast”. They also noted that given concerns of breast cancer overtreatment, we need to modify our approach. They pointed out that MRI might be useful in developing individualized treatment approaches, such as multiple lumpectomies if more than one cancer is found (instead of mastectomy). They appropriately called for more research to determine how preoperative breast MRI should best be utilized.
The post Preoperative Breast MRI appeared first on Dr Deanna Attai.
]]>The post Increasing Mastectomy Rates – Science vs. Personal Choice appeared first on Dr Deanna Attai.
]]>This past weekend, I gave a talk at the Southern California Chapter of the American College of Surgeons Annual Meeting – the title of the talk was Increasing Mastectomy Rates – Science vs. Personal Choice.
There is a tremendous amount of literature documenting the increasing mastectomy rates. The talk focused on women with early stage breast cancer at average risk for developing a recurrence or new cancer – women without a BRCA gene mutation. As has been my practice for several years when giving a talk which includes the patient experience, I asked you for input, and received a lot of information. The following is a summary of the talk, including your perspective.
The use of mastectomy for breast cancer has been documented as early as the 1500s, despite the fact that general anesthesia did not come into use until the 1840s. Sir William Halsted described the radical mastectomy, which involved removal of the breast, all of the overlying skin, the pectoral (chest) muscle, and a significant number of lymph nodes. It was a very aggressive surgery but at the time, many women at the time presented with advanced disease – cancers that grew through the skin or chest muscle. The Halsted theory was that if the breast and lymph nodes could be removed with an extensive “en bloc” surgery, the cancer had a lower likelihood of spreading. However, despite this aggressive approach, the dismal survival rates from breast cancer did not improve.
Halsted died in 1922, but the radical mastectomy remained the surgical procedure of choice until the 1960-70s. The landmark NSABP B04 trial, led by Dr. Bernard Fisher, demonstrated that regardless of surgical decision (radical mastectomy vs. total mastectomy – no removal of the muscle) the survival rates were equivalent, and these results have held up for 25 years(1). The Fisher theory was that cancer may be metastatic from the beginning, and that a more extensive surgical procedure would not be expected to improve survival rates. The NSABP B06 trial demonstrated equivalent survival rates whether women underwent mastectomy, lumpectomy / radiation, or lumpectomy alone. However, if radiation therapy was not performed, the risk of local recurrence (cancer returning in the breast) was 39.2%, compared to 14.3% with radiation(2). This is the basis for our current recommendation of lumpectomy followed by radiation therapy for early stage breast cancer. A 1990 NIH consensus panel stated that “breast conservation treatment is an appropriate method of primary therapy for the majority of women with early-stage breast cancer and is preferable because it provides survival rates equivalent to those of mastectomy while preserving the breast’’(3).
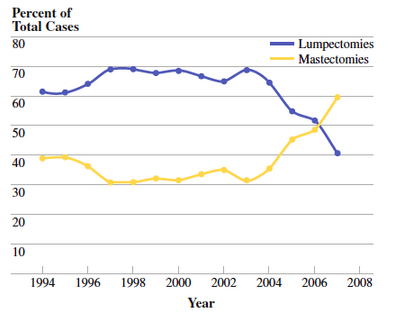
This was seen as a major scientific advance, and one that was embraced by patients – no longer did women need to have a breast removed for early stage disease, and from the early to mid 1990s, lumpectomy rates started increasing while mastectomy rates decreased.
The Women’s Health and Cancer Rights act of 1998 stated that if an insurance company covered the procedure of mastectomy, they were required to cover reconstructive surgery, including procedures performed on the other breast to produce a symmetrical appearance, as well as prosthetics for lymphedema. This set the stage for immediate reconstruction, which prior to this time was generally not performed (or recommended) on a regular basis.
We think of the “Celebrity Effect” when we hear Angelina Jolie, Amy Robach, and others discuss their decisions. But in 1987, Nancy Regan underwent a mastectomy for breast cancer, and she received a significant amount of criticism for her decision, both from the medical community as well as from advocacy groups. Women who underwent breast cancer surgery from the end of 1987 to early 1988 were 25% less likely to undergo lumpectomy compared to earlier in 1987, prior to her diagnosis(4). Lumpectomy rates subsequently increased, but she later wrote “This is a very personal decision, one that each woman must make for herself. This was my choice, and I don’t believe I should have been criticized for it”(5).
Around 2004, it was noted that mastectomy rates started rising(6). This trend was seen nationally as well as in many individual institutions.
In addition to an increase in mastectomies being performed for early stage breast cancer, an increase has been seen in contralateral prophylactic mastectomy – removal of the other, non-cancerous breast. Many studies have been published confirming this trend, and also evaluating factors associated with an increased mastectomy rate(7,8,9). They include:
– Young age, Caucasian race
– Higher economic status, better insurance, availability of reconstruction
– Family history of breast cancer or genetic testing – even if the genetic testing was negative
– Undergoing an MRI, even if the MRI was normal
Patient factors have also been evaluated. Many studies have cited that women make their decisions out of fear. Interestingly, there seems to be some intellectual disconnect – women report that they understand there is no improvement in survival, yet state that they made their decision “to live longer”. The physician has been identified as a very important source of information, yet only 1/3 of women stated that a desire to follow their physician’s recommendation was important in making their decision. Many women over-estimate their risk of developing a new breast cancer – some reporting they think their risk is as high as 50%. Other studies have reported that women make their decisions to gain a sense of control over cancer, but that many have an exaggerated sense of control, stating that they are making the decision “so I don’t have to go through this again”, while admitting that they are aware that mastectomy does not reduce the rate of metastatic disease. The impact of a family member / friend experience was also noted to be very important. All of us make decisions in our daily lives based on personal experience rather than hard facts – a woman facing a decision about breast cancer surgery is no different. Finally, many woman remain very satisfied with their decision even 20 years after the surgery. However, it is important to note that 10-30% report issues related to self-esteem, body image, sexuality, emotional stability, and overall quality of life (10, 11, 12).
Some facts(10, 13, 14, 15):
– For women at average risk of breast cancer (BRCA negative) the rate of developing a new breast cancer is approximately 0.5 – 0.75% per year. This can be reduced if the women undergoes chemotherapy and/or endocrine therapy
– Mastectomy for early stage breast cancer or contralateral prophylactic mastectomy does not reduce the likelihood that breast cancer will metastasize (spread to other areas of the body)
– The complication rate increases with more surgery – bilateral mastectomy is associated with 30-40% risk of complications including infection, fluid accumulation, and re-operation.
So what did you, the #BCSM Community have to say? Out of those who responded:
– “I knew survival rates were the same” – most patients well informed, had surgeons who presented all sides, supported their decision
– 40% said decisions influenced by family/friend experience
– 15% had lumpectomy initially, then opted for bilateral mastectomy after anxiety of repeat imaging and biopsies.
– 6 patients: lumpectomy and radiation: significant problems with wound healing, fibrosis and later underwent a mastectomy
– 5 patients subsequently developed metastatic disease; no regrets on their decision
– 3 patients required multiple surgeries due to revisions, infection, lost implant – no regrets
– 2 patients felt pushed into their decision, one by family members and another by their physician – both regretted their decision
There are a lot of comments on the original blog post; here are a few I received by email:
– “I wish doctors, researchers and the media understood (some do) – there are many valid reasons for choosing a mastectomy, even with the state-of-science today”
– “The focus is on ‘simple’ surgery – the potential toxicity of radiation therapy is grossly minimized. While serious and long-term side effects of radiation therapy may be rare, they do occur. It is ironic now that patients have a choice in treatment selection, there is so much hand-wringing by the medical establishment in the choices that many women make”
– “We are diligent. We are thoughtful. We have good reasons for choosing the “big surgery”. Our doctors explain the risk factors, we process the information, we understand the full ramifications of our choice, and are still confident that this is the right choice for our set of circumstances.
– It may not fit the medically necessary criteria, but it may fit with the emotionally necessary criteria. I hear your evidence based science and I’ll raise you five intangibles…”
So what is the answer? Clearly physicians have a responsibility to educate our patients not only on the lack of overall survival benefit, on the complication rates. Physicians also need to do a better job of assessing and explaining a patient’s risk of developing a recurrence or a new breast cancer. And patients should be encouraged to take their time, obtain opinions, and carefully consider all options prior to making a decision. But rather than irrational fear, what many of see in our practice is “Reasonable Fear”. Patient’s biases and personal experiences need to be acknowledged. Some bias, but not all, can be overcome with education. But until science advances to allow us to truly predict who will and will not develop a recurrence or a new breast cancer, personal choice should remain an option.
References:
1. Fisher B et al. 25 Year follow up of a randomized trial comparing radical mastectomy, total mastectomy, and total mastectomy followed by irradiation. NEJM 2002;347 (8)
2. Fisher B et al. 20 Year follow up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer NEJM 2002;347 (16)
3. NIH Consensus Conference: Treatment of Early Stage Breast Cancer. JAMA 1991 265
4. Nattinger AB, et al Effect of Nancy Regan’s mastectomy on choice of surgery for breast cancer by US women. JAMA 1998 (279) 10 762-766
5. Olson, J: “Bathsheba’s Breast: Women, Cancer and History” The Johns Hopkins University Press 2002
6. McGuire KP, et al Are mastectomies on the rise? A 13 year trend analysis of the selection of mastectomy versus breast conservation therapy in 5865 patients. Ann Surg Oncol 2009 16:2682-2690
7. Mahmood U, et al Increasing national mastectomy rates for the treatment of early stage breast cancer. Ann Surg Oncol 2013 20:1436-1443
8. Yao K, et al Trends in contralateral prophylactic mastectomy for unilateral cancer: A report from the national cancer database 1998-2007. Ann Surg Oncol 2010(17) 2554-2562
9. King TA, et al Clinical management factors contribute to the decision for contralateral prophylactic mastectomy. J Clin Oncol 29:2158-2164 97-200
10. Rosenberg SM, et al Perceptions, knowledge and satisfaction with contralateral prophylactic mastectomy among young women with breast cancer Ann Intern Med 2013;159:373-381
11. Covelli AM, et al ‘Taking control of cancer’: Understanding women’s choice for mastectomy. Ann Surg Oncol DOI 10.1245/s10434-014-4033-7
12. Frost MH, et al Contralateral prophylactic mastectomy: Long term consistency of satisfaction and adverse effects and the significance of informed decision making, quality of life, and personality traits. Ann Surg Oncol 2011 18:3110-3116
13. Fayanju O et al Contralateral prophylactic mastectomy after unilateral breast cancer: a systematic review and meta-analysis. Ann Surg 2014; 260:1000-1010
14. Roberts A et al Cost effectiveness of contralateral prophylactic mastectomy for prevention of contralateral prophylactic mastectomy. Ann Surg Oncol 2014 21:2209-2217
15. Miller ME et al Operative risks associated with contralateral prophylactic mastectomy: A single institution experience. Ann Surg Oncol 2013 204113-4120.
The post Increasing Mastectomy Rates – Science vs. Personal Choice appeared first on Dr Deanna Attai.
]]>The post Misconceptions and Fears Prompt Contralateral Mastectomies appeared first on Dr Deanna Attai.
]]>The following article appeared in Medscape and covered a recent study suggesting that many women base their decision to undergo a mastectomy on fear. I was happy to contribute my thoughts to what is a very complex issue and a very difficult decision for so many women. ~DJA
Fran Lowry
Sep 16, 2013
Women with breast cancer, especially younger women, are choosing to have their healthy breast removed because of mistaken beliefs about the effectiveness of mastectomy and unfounded fears about the risks for contralateral disease.
In a cross-sectional survey of 123 women with early bilateral breast cancer who chose to undergo contralateral prophylactic mastectomy (CPM), the overwhelming majority cited improving their chances of survival (94%) and reducing the risk that cancer will develop in the other breast (98%) as their primary reasons for deciding to have the additional surgery.
The results appear in the September 17 issue of the Annals of Internal Medicine (Ann Intern Med. 2013;159:428-429).
The findings highlight the need for doctors to take the time to explain the true risks and benefits of CPM, Pamela R. Portschy, MD, and Todd M. Tuttle, MD, from the University of Minnesota in Minneapolis, Minnesota, write in an accompanying editorial.
The 10-year cumulative risk for contralateral breast cancer is only 4% to 5%, the editorialists note, citing other research. In addition, “CPM is not likely to improve breast cancer survival rates.”
“The apparent discordance between patient perceptions and realistic expectations provides a teachable opportunity for physicians treating newly diagnosed patients with breast cancer,” the editorialists write, adding that the women in the study identified physicians as the most important source of information about CPM.
The study authors do not want their participants to be judged for their beliefs. “The purpose of our study was not to pass judgment on these women, because for some, for example those with BRCA mutations, it may be the right decision,” lead author Shoshana M. Rosenberg, ScD, MPH, from the Susan F. Smith Center for Women’s Cancers at the Dana-Farber Cancer Institute in Boston, told Medscape Medical News.
“Our aim was to really understand why women are deciding, in greater and greater numbers, to have this surgery,” she explained.
Nonetheless, there is more at stake for these women than just undergoing an extra surgery.
A recent study of 4200 breast cancer patients, presented at the annual meeting of the American Society of Breast Surgeons in May, found that women opting for CPM had twice as many postoperative complications as those opting for a single mastectomy.
Doctors Are Most Important Sources of Information
In their study, Dr. Rosenberg and her team surveyed 123 women from 8 academic and community hospitals in eastern Massachusetts who had early-stage cancer in 1 breast but who elected to have both of their breasts removed.
The women were part of a larger cohort study of 550 women diagnosed with early-stage breast cancer in 1 breast only from November 2006 to November 2010.
All the women were 40 years of age or younger at the time they were diagnosed; 26% had a first-degree relative and 62% had a second- or third-degree relative who had been diagnosed with breast or ovarian cancer. About one quarter of the women had a BRCA1 or BRCA2 gene mutation.
A 23-item questionnaire was administered to the women who reported having a bilateral mastectomy. They were asked how they made their decision to have bilateral mastectomy and about their knowledge, perception of risk, and breast cancer worry.
The vast majority (95%) said that the decision to remove the healthy breast gave them peace of mind.
The women also reported that doctors were their most important source of information when they were making their decision. More than half of the respondents (68 women) indicated that they were the first to bring up the issue of CPM. Half of the women reported that their physicians discussed reasons not to have the surgery.
A third of women reported that the number of surgeries or procedures needed was higher than they expected, and 42% reported that their sense of sexuality was worse than they expected after surgery. A similar percentage of women reported that they felt self-conscious about their appearance.
Removing the healthy breast might be the right decision for some women, Dr. Rosenberg emphasized. “But,” she said, “we want to make sure they are making this decision in a setting where it’s informed, and also where they are supported. Obviously, when you get a breast cancer diagnosis, it’s a very anxious time; there are a lot of worries, fears, and concerns. We think these issues should be addressed. The decision-making process needs to be supported.”
Women Not Making Well-Informed Decisions
In an interview with Medscape Medical News, Dr. Tuttle, one of the editorialists, said he is very concerned that women do not appear to be making well-informed decisions about their care.
“Many women have unrealistic expectations of what having their opposite breast removed will do,” he said.
“We did a study that was published last year in which the women we interviewed thought their average risk of getting cancer in the opposite breast over 10 years was more than 30%, when the actual risk is about 4% to 5%. The take-home message from this study, which is a great study, is that physicians need to take time and explain the facts to their patients.”
Dense Breasts a Factor?
The decision-making process for women newly diagnosed with breast cancer is extremely complex, according to Deanna J. Attai, MD, a surgeon and director of the Center for Breast Care in Burbank, California.
Physicians might wonder why so many women are choosing CPM or even mastectomy for early-stage cancer, but their patients do provide some answers, Dr. Attai told Medscape Medical News.
“There is no question that many women make their decision based on fear and an inflated sense of risk,” she said.
Dr. Attai pointed out that most of the women felt that the worry that subsequent screenings would fail to detect a contralateral breast cancer was a very important factor in making their decision, but she noted that this was not stressed by the study authors.
“Personally, I think this is a big factor. This study evaluated women under 40. There is no question that most women under 40 have relatively dense breast tissue, and there is no question that mammography is less sensitive in these women. Many younger women detect their breast cancer when it is palpable,” she said. “If your cancer was not picked up on a mammogram, you have very little faith that future mammograms would be helpful in detecting a contralateral cancer.”
Dr. Attai also said that a 40-year-old woman’s risk of developing a contralateral breast cancer could be more than 20%, assuming that she lives to age 80. But, “with chemotherapy and endocrine therapy, that risk can be less than 10%,” she added.
Dr. Attai said that breast cancer surgeons attempt to present all of the facts about surgery to their patients. “We tell them that the potential complication rate of the surgery can be as high as 50%, including the issues of unplanned operations, less than ideal cosmetic results, sexual side effects, and self-image issues,” she explained. “I also tell my patients that a 10% to 20% risk of developing a contralateral breast cancer also is an 80% to 90% chance of not developing a contralateral breast cancer.”
Dr. Attai said she is very direct with patients who come into her office initially saying they want a CPM.
“I tell them they need to hear me out while we discuss the realities of no increased survival, overestimation of risk, and so on,” she said.
One Real-World Example
Dr. Attai offered the following recent example from her practice.
“The patient is in her early 40s and her stage I breast cancer was detected on a screening mammogram. She came to me wanting bilateral mastectomy. She had seen 2 other breast surgeons and had opinions from 3 plastic surgeons,” Dr. Attai recounted. The patient was “well-informed” about the lack of survival benefit, the low risk of developing a contralateral breast cancer, and the potential complications (including self-image, sexual) of this surgery.
However, 2 of the patient’s friends had been treated for breast cancer with lumpectomy and radiation, and their experiences colored the patient’s outlook. “One was diagnosed with a contralateral breast cancer 18 months later, and then opted for bilateral mastectomy. She had horrible problems with healing on the radiated side and underwent 2 or 3 other procedures,” Dr. Attai explained. “The other friend had a lumpectomy and radiation and has a severely contracted treated breast, which is very hard and fibrotic. She has seen multiple reconstructive surgeons who have informed her of the complexity of her case and that any attempt at reconstruction is likely to result in several procedures.”
“None of these women have a family history of breast cancer or are BRCA positive. My patient told me today that she knew she made the right decision for herself, and the experience of her friends reinforced that,” Dr. Attai said.
“No matter how much we educate patients, we cannot take away their personal experiences. Because breast cancer is so common, everyone knows someone who has been treated, and there are always horror stories. I think acknowledging and discussing a patient’s personal experiences and biases is extremely important. Some of that can be overcome by education, but not all,” she added.
Dr. Rosenberg, Dr. Tuttle, and Dr. Attai have disclosed no relevant financial relationships.
The post Misconceptions and Fears Prompt Contralateral Mastectomies appeared first on Dr Deanna Attai.
]]>