24 April 2020
A new drug was recently approved by the US Food and Drug Administration (FDA) for the treatment of metastatic breast cancer – breast cancer that has spread to other areas of the body, such as the bones, liver, lungs or brain. Sacituzumab govitecan (Trodelvy), which is given by intravenous infusion, was granted accelerated approval to treat metastatic triple negative breast cancer in patients who have already been on 2 prior treatments for their disease.
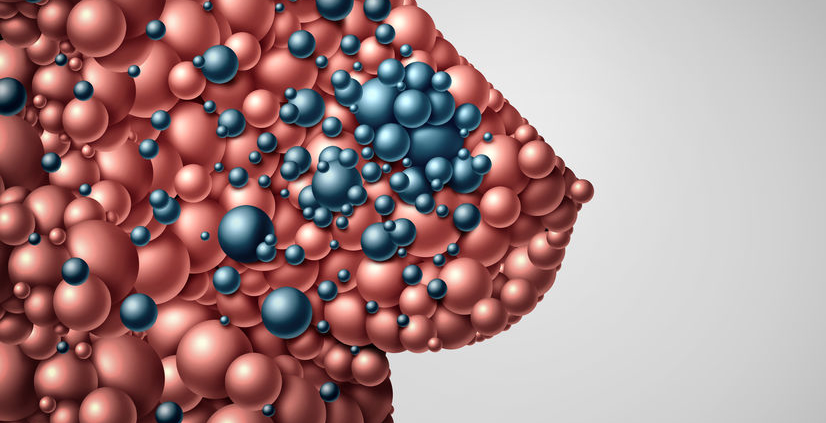
Triple negative breast cancer accounts for approximately 15% of breast cancers. It is more common in younger patients, African Americans, and those with a BRCA1 gene mutation. It can be very challenging to treat since there is no specific cellular target, such as the estrogen receptor or Her2/neu protein. Patients with triple-negative breast cancer very commonly receive chemotherapy but the disease may come back or progress despite aggressive treatment.
Sacituzumab govitecan is an antibody-drug conjugate, which is an antibody that is combined with a chemotherapy drug. The antibody targets a protein (trophoblast cell surface antigen-2, or trop-2) on the surface of the cancer cell, and the chemotherapy drug causes breaks in the tumor cell DNA, which leads to cancer cell death. The FDA approval was based on a non-randomized (meaning all patients received the study drug) study of 108 patients who were experiencing disease progression despite receiving between 2 – 10 prior treatment regimens. Among the study participants, approximately 33% experienced a partial or complete tumor response to the medication. Median duration of treatment response was nearly 8 months. Severe adverse reactions included diarrhea, neutropenia (low white blood cell counts), anemia (low red blood cell counts), fatigue, nausea and vomiting. 2 patients stopped treatment due to side effects.
Any advance in the treatment of metastatic breast cancer is welcome news. It is hoped that as new drugs are developed, a longer-lasting response to therapy will be achieved.
Additional Information: