7 June 2020
An abstract presented at last week’s virtual meeting of the American Society of Clinical Oncology focused on whether or not there is a benefit to surgery for the primary breast tumor in patients with metastatic, or Stage IV, breast cancer.
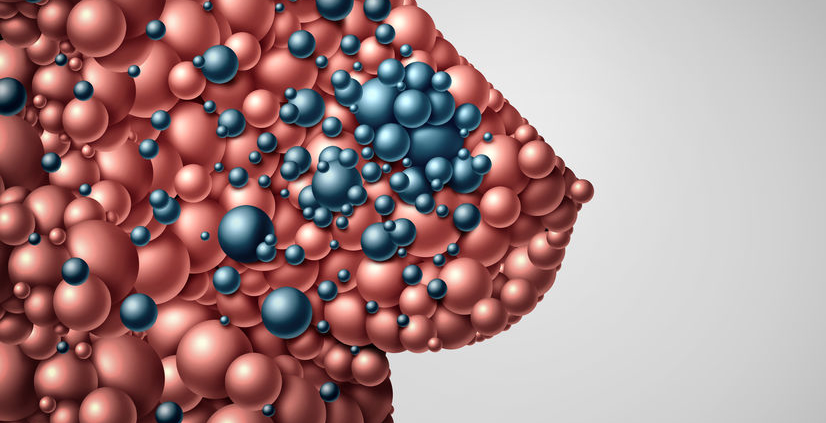
Metastatic breast cancer (Met-BC) is when the breast cancer spreads beyond the breast and underarm lymph nodes. Common sites of metastases include the lungs, liver, bones, and brain. Anyone diagnosed with breast cancer has the potential to develop metastatic disease, but approximately 5-10% of patients are found to have Met-BC at the time of initial diagnosis, known as de-novo Stage IV. For these patients, it has been controversial whether or not to recommend some form of breast surgery (lumpectomy or mastectomy) to remove the primary tumor. Some studies have shown a survival benefit when the primary tumor is removed, but widespread adoption of the results of these studies has been limited because in many of these studies, patients who underwent surgery were younger, healthier, and had a lower volume of metastatic disease compared with the general population of patients with Met-BC.
Dr. Seema Khan presented the results of the ECOG-ACRIN Research Group E2108 study. In this study, patients who had stable Met-BC (after 4-8 months of treatment) were randomized to either surgery or no surgery for the primary tumor. The two study groups were well-matched for age, race, and breast cancer subtype. With a median follow up of 59 months, there was no improvement in overall survival or in progression-free survival. Local progression (cancer continuing to grow in the breast) was more common in patients who did not undergo surgery (25.6 versus 10.2% at 3 years). At 18-month assessment, health-related quality of life was significantly worse in those who underwent surgery, but no differences were observed at the 6-month or 30-month assessment intervals.
During her presentation, Dr. Khan acknowledged that there may be situations where surgery for the primary tumor is a reasonable option in the setting of Met-BC. She noted that there is room for individualization, but stressed that as there is no survival benefit and no improvement in quality of life, surgery for the primary tumor in the setting of Met-BC should not routinely be performed.
It is important to note that any medical meeting abstract, whether an oral presentation or poster, has been evaluated by the meeting program committee but has not been subject to rigorous peer review as would occur with a formal manuscript submission. Abstracts often do not include the full set of results, and additional findings may be included in the eventual publication, some of which may be different than those presented in the abstract. We look forward to the peer-reviewed publication when it is available.