23 August 2016
A study published in the Annals of Internal Medicine evaluated screening mammography taking into account breast density and breast cancer risk. For women age 50-74, the conclusion of the authors was that for women of average risk with low breast density (fatty or scattered fibroglandular), triennial (every 3 year) mammography screening averted the same number of breast cancer deaths as annual or biennial screening. Women screened every 3 years also had lower rates of biopsy procedures. For women at high risk with high breast density (heterogeneously or extremely dense), annual screening was better. High risk / high density patients accounted for approximately 1% of the study population.
The study was funded by the National Cancer Institute. The authors used simulation modeling which included national breast cancer incidence, breast density, and screening performance data. They did not include patients with genetic abnormalities such as BRCA 1/2 mutations. They also did not take into account the impact of MRI or tomosynthesis / 3D mammography.
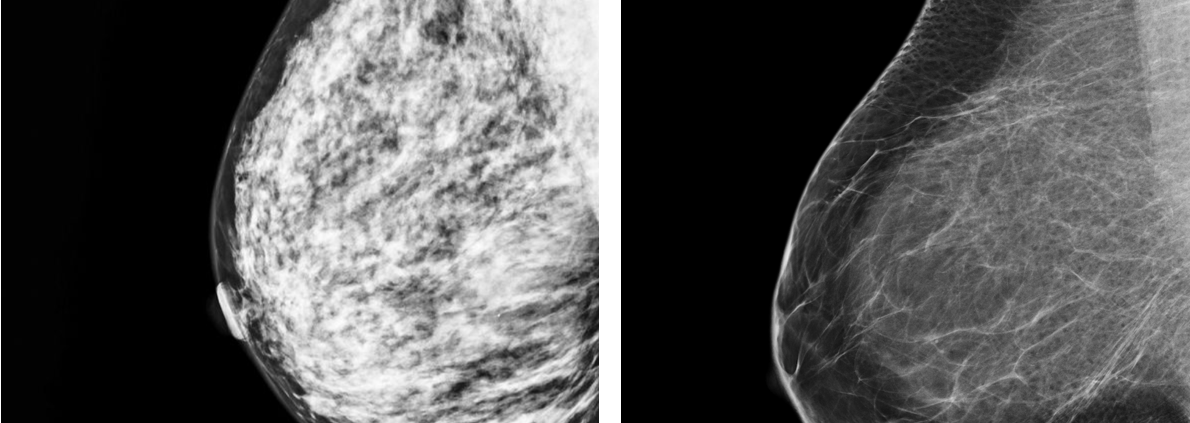
Risk assessment involves a calculation (using various models) which takes into account a woman’s age, body mass index, menstrual and reproductive history, family history, prior biopsies, and other factors known to influence the risk of breast cancer development. In the current study, the authors used a risk calculator that takes into account breast density. Breast density is a factor associated with breast cancer, although studies vary regarding the impact of density on risk. Adding to the confusion, breast density rating is subjective – different radiologists may assign different density scores to the same patient. The model used in the current study also takes into account factors such as improved detection using digital mammography, improved treatment effectiveness, and the usual decrease in breast density that is seen with increasing age. It is unclear at this time which is the “best” risk assessment model to use – all have limitations, some significantly over-estimate risk, and none are a “crystal ball”.
So what should women do? The ideal screening test is one that is inexpensive, readily available and safe. It should also find cancers early enough to make a difference. Mammograms are an imperfect tool but they perform reasonably well in a wide variety of settings. The ideal screening program is to tailor the technology and screening frequency to the patient’s risk – one size never fits all. Women should be aware of their family history and risk factors, ask about their breast density, and then discuss these factors as well as their personal preferences regarding breast cancer screening with their physicians. True individualized and personalized risk-based screening is not yet a reality, but by making recommendations based on risk, we are taking steps in the right direction.