** 6 December 2018 – Editor’s Note:
The NSABP B-39 clinical trial results were recently presented at the San Antonio Breast Cancer Symposium. This study compared 3 forms of radiation therapy. After 10 year followup, approximately 4% of patients who underwent whole-breast irradiation after lumpectomy developed cancer recurrence in the same breast. This is lower than what was quoted below (10-15%, point #3) which was based on older data. This new study demonstrates that the recurrence rate after lumpectomy and radiation (4%) is nearly equivalent to that of mastectomy (1-3%).
3 June 2014
A study was recently published evaluating the reasons why women diagnosed with breast cancer might undergo a contralateral prophylactic mastectomy. First, some definitions:
– Mastectomy – removal of the entire breast
– Prophylactic mastectomy – removal of a breast that does not have cancer
– Contralateral prophylactic mastectomy (CPM) – removal of the breast that does NOT have cancer, in a patient undergoing mastectomy for cancer on the other side
The study, which was published in JAMA Surgery, concluded that “Many women considered CPM and a substantial number received it, although few had a clinically significant risk of contralateral breast cancer. Receipt of magnetic resonance imaging at diagnosis contributed to receipt of CPM. Worry about recurrence appeared to drive decisions for CPM although the procedure has not been shown to reduce recurrence risk. More research is needed about the underlying factors driving the use of CPM.”
Some background information:
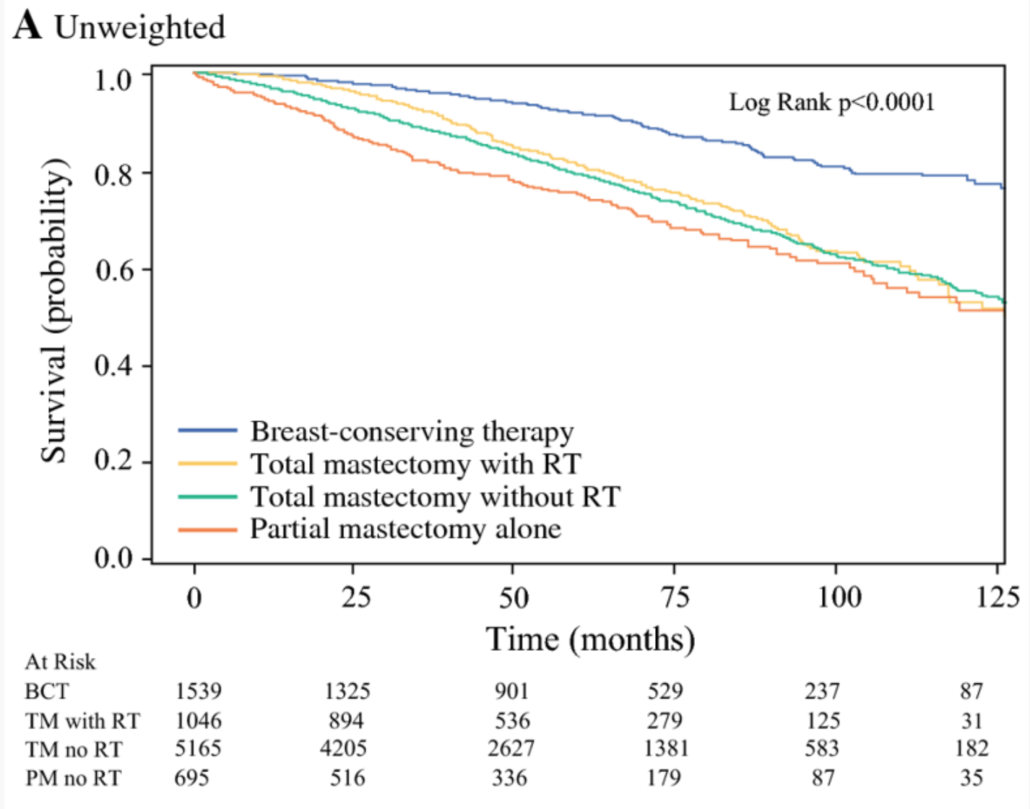
1. Over 25 years’ worth of data exists showing that long-term survival is equivalent whether a woman undergoes a lumpectomy or a mastectomy: In other words, you will not live any longer if your breast is removed.
2. There is no difference in the likelihood of metastatic disease (spread outside the breast – most commonly bones, liver, lung and brain) whether you have a lumpectomy or mastectomy.
**see editor’s note, above.
3. Lumpectomy followed by radiation therapy (this is also called breast conservation therapy, or BCT) generally has low rates of “in breast recurrence” or “in breast new primary” – low rates of the original cancer coming back in the same breast, or a new cancer developing in the same breast. These rates are historically about 10-15%, although these rates are likely reduced with modern adjuvant antihormonal, radiation, and chemo- therapies.
4. Even though much more breast tissue is removed (~99% of breast tissue cells) mastectomy is still associated with a 1-3% risk of cancer recurrence at the site of breast removal. This is usually in the skin or muscle.
5. CPM is associated with a 20-40% complication rate, especially unplanned additional surgery
6. The average woman’s risk of developing a new cancer in the opposite breast is approximately 0.5-1% per year. If a cancer develops in the contralateral (other) breast, it is considered a “new primary” – a whole new breast cancer. Even though it might be the same type as the original cancer, it is generally not considered a recurrence. If the original cancer is estrogen / progesterone receptor positive, taking tamoxifen or aromatase inhibitors can reduce the risk of cancer returning after a lumpectomy, and can reduce the risk of a new cancer developing in the other breast. However, lumpectomy or mastectomy for the original cancer does not alter the rate of new breast cancer development.
7. Women who carry a BRCA gene mutation have a 60-80+% lifetime risk of developing breast cancer in either breast, and a high risk of developing a new breast cancer, so bilateral mastectomy is often recommended. These patients are generally excluded from the discussions regarding whether or not CPM is a reasonable option due to their extremely high risk.
Over the past 20 years, research studies have supported a “less is more” approach to breast cancer surgery such as: BCT, narrower margins of normal tissue removed around cancer, and less extensive lymph node removal. Before instituting these changes, studies were done to ensure that less aggressive surgery does not impact long-term survival rates. Despite these advances, there has recently been a steady increase in the rate of mastectomy, as well as CPM. In article after article, physicians are scratching their heads. The use of MRI, inadequate education, unrealistic expectations from reconstructive surgery, the “celebrity effect”, as well as fear and anxiety have been blamed.
The “new” study and our thoughts:
The recent study in JAMA Surgery focused on a small subset of women (8%) from a national database that elected CPM as part of treatment for unilateral breast cancer. The authors reported that of 106 patients who received CPM, “80% indicated it was done to prevent breast cancer from developing in the other breast,” leaving only 21 patients (1.5%) from their sample of 1447 surveyed women that elect CPM for reasons other than the prevention of the development of a new contralateral breast cancer. However, the author’s conclusions ignore this and direct the reader’s attention instead to patients’ concern for recurrence, stating, again, that “worry about recurrence appeared to drive decisions for CPM.”
The problem with this type of analysis is this: when ‘patient fear’ is discussed, it frequently is implied by the reporting media that hysterical women are running to the operating room to be unnecessarily operated on by uneducated surgeons.
Judging the merits of a surgical procedure or treatment on the fact that few women “are likely to experience a survival benefit,” is not reflective of the complexity of the treatment decision-making process for women with a new diagnosis of breast cancer. Faced with a multitude of decisions to make in a short time frame, it is not surprising that many such patients will report anxiety concerning recurrence.
The truth is simple: surgical choice is a combination of factors. There is little doubt that some physicians do not spend the time needed to hear the concerns of their patients and respond to them appropriately. Conversely, some patients do not want to hear all of the facts, preferring simply to opt for what seems the “safest” approach, even though the science says otherwise.
What we see in our offices is a rational fear: Many women understand that the type of surgery does not determine their survival. While of utmost importance, survival is not the only thing that is important to women being treated for breast cancer. Women worry about having to repeat the whole process in another year or so if something new shows up on a mammogram or if a lump is felt. Women question the value of annual mammography for surveillance when their initial tumor was not picked up by a mammogram. Women have seen their family members and friends develop complications from radiation therapy and from attempts to perform additional surgery after radiation therapy. While women understand that a mastectomy is no guarantee that they will remain cancer-free, to many it is such a significant decrease in the rate of recurrence or new primary cancer that they feel it is an acceptable trade off for the complication rates that have been reported in patients who undergo a CPM with reconstruction. Physicians also agonize over the decision. Properly educated patients are in the best position to make decisions regarding their own breast health care, but even the best education does not alleviate all anxieties, nor can it eliminate all risk.
Physicians and researchers talk about the increasing rate of CPM as a crisis. But the real crisis is that at this point, we simply do not have options for women that they are comfortable with. Unnecessary surgery is a concern for patients and physicians. However, until we can look a woman in the eye and give her more accurate information about her individual risk of recurrence or new primary disease, it is our opinion that the decision for CPM should be between a woman, her family, and her physicians.
Additional Reading:
JAMA Editorial: Contralateral Prophylactic Mastectomy – An Opportunity for Shared Decision Making
Medscape Article – Misconceptions and Fear Prompt Contralateral Mastectomy
The Patient Perspective: Blog Post by Catherine Guthrie
Deanna J. Attai, MD
Michael S. Cowher, MD