12 January 2021
12 January 2021
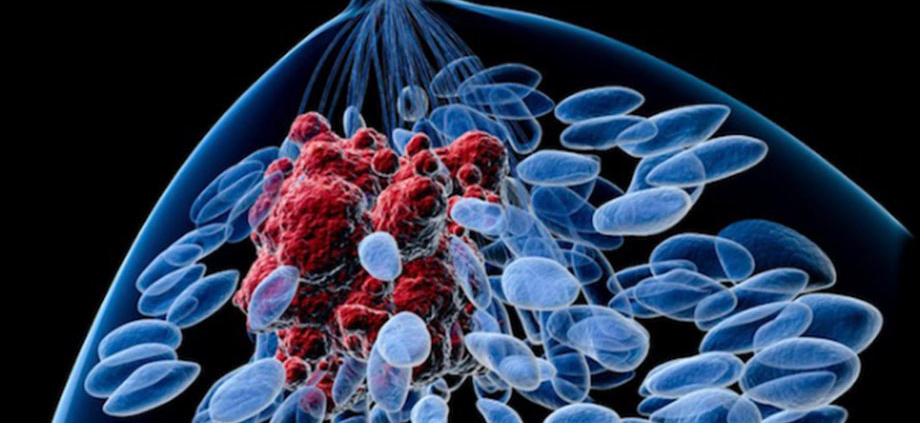
The National Cancer Institute (NCI) recently announced that they will start tracking breast cancer recurrence. Currently, initial cases of breast cancer are reported, but local / regional (in the breast or underarm lymph nodes) or metastatic (elsewhere in the body, most commonly lungs, liver bones and brain) breast cancer recurrences are not. It is unclear how many patients with early stage breast cancer experience a recurrence, although it has been reported to be approximately 30%.
It will be several years before we see meaningful data, but this is most certainly a step in the right direction. Patients and physicians alike are frustrated by the lack of reliable data on recurrence rates. Patients who develop metastatic cancer are frustrated that they are not “counted.” And much credit to Katherine O’Brien, a woman in Chicago who is living with metastatic breast cancer – she led the creation of a change.org petition, which collected nearly 12,000 signatures, requesting that federal and state registries begin collecting this information.
This most certainly is a step in the right direction to ensure that all cases of breast cancer, both initial and recurrent diagnoses, are captured. It’s also a testament to the power of the patient advocate!