28 November 2019
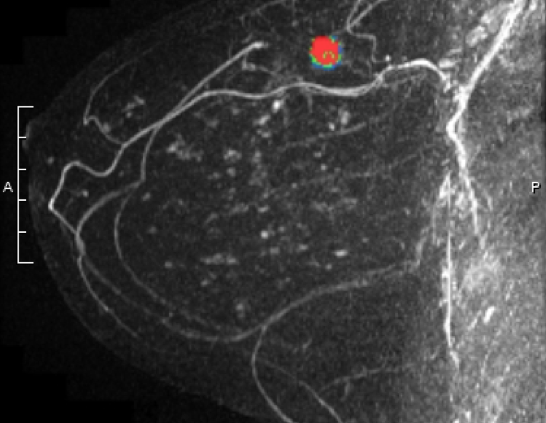
A study recently published in the New England Journal of Medicine* suggests that the use of breast MRI in addition to mammograms in women with extremely dense breast can improve the rate of “interval cancer” detection.
Interval cancers are those that occur after an apparently normal mammogram, but prior to the next scheduled mammogram. An example could be a lump felt by a patient a few months after a “clear” mammogram. Interval cancers are more likely to be more aggressive (triple negative or Her2/neu over-expressed) and/or occur in women who have dense breasts on mammogram.
Researchers in the Netherlands evaluated the role of breast MRI as a supplemental screening tool in women age 50-74, who had a normal mammogram and an “extremely dense” (BIRADS 4 density) reading. After a normal mammogram, women were randomized 1:4 to supplemental MRI versus continued mammogram only (1 woman received an invitation for MRI for every 4 who continued undergoing only mammograms). The standard mammography screening in the Netherlands is every 2 years. 8061 women were in the “intent to treat” with MRI group and 32,312 in the mammogram alone group. 59% (4783) of women randomized to the MRI group actually accepted and underwent supplemental MRI.
Some of the key findings:
- In the MRI “intent to treat” group, they found 2.5 / 1000 interval cancers and in the mammography group there were 5.0 / 1000 interval cancers
- However, out of the 20 interval cancers discovered in the MRI “intent to treat” group, only 4 were in women who had actually undergone MRI. The other 16 were in women were randomized to the MRI group but did not have the study – they had mammograms only
- Out of the women who underwent MRI, approximately 10% (454) were recalled for additional imaging
- 300 women had needle biopsies due to findings on MRI, and out of those, 79 (26%) were found to have cancer. 64 of the cancers were invasive and 15 were noninvasive (DCIS). 74% of the biopsies did NOT show cancer
- The cancers detected by MRI on average were smaller than those detected by mammography. The majority were hormone receptor positive and lymph node negative
- DCIS was more likely to be detected in women undergoing MRI (0.31%) versus mammogram alone (0.03%)
- 0.1% of patients who had an MRI experienced an adverse reaction including fainting, contrast (dye) reaction, and issues with the intravenous line
- The study was NOT designed to determine if MRI improved the survival rates from the cancers detected.
Some important points were raised in the accompanying editorial by Dr. Dan Longo*. He noted that with any screening test, the goal should be that early detection of the cancer results in a higher likelihood of cure but admitted that any screening test is associated with false positives, and many patients with an abnormal test will not have cancer. He also noted that an “imprecisely defined fraction of cancers that are detected by screening do not progress to cause symptomatic disease or to kill the patient” but that “our dilemma is that for most tumors we cannot tell the difference between cancers that can kill you and those that cannot.”
The study focused on patients with extremely dense breasts, which the authors estimate account for approximately 10% of patients undergoing mammograms. It is not clear if these findings would be similar in patients with level 3 breast density (heterogeneously dense), those undergoing tomosynthesis (3D) mammograms, or in patients who are undergoing mammograms every year. They did not stratify patients by risk assessment and it’s important to note that while dense breasts are a risk factor for breast cancer, not all women with dense breasts are considered “high risk”. US national guidelines currently recommend supplemental imaging with MRI in patients who have a lifetime risk of breast cancer of 20% or greater as calculated by a risk assessment model. Due to high recall and false positive rates associated with MRI as well as possible concerns related to the contrast material, we do not currently recommend MRI for all women, or even for all women with dense breasts.
As one of their concluding statements, the authors did note that the 10% recall rate “is a concern for potential implementation of supplemental screening” [with MRI]. This study adds to the body of literature regarding cancer detection in women with dense breasts, but Dr. Longo concluded in his editorial: “… will we be putting these women at increased risk of procedures without contributing to their eventual survival?” Going forward, it will be important to look at ways to decrease false positive results and costs of supplemental imaging, as well as evaluate whether or not outcomes are improved by additional testing.
*If you are not able to access the full study and would like a copy, please email me: contact at drattai dot com