5 December 2015
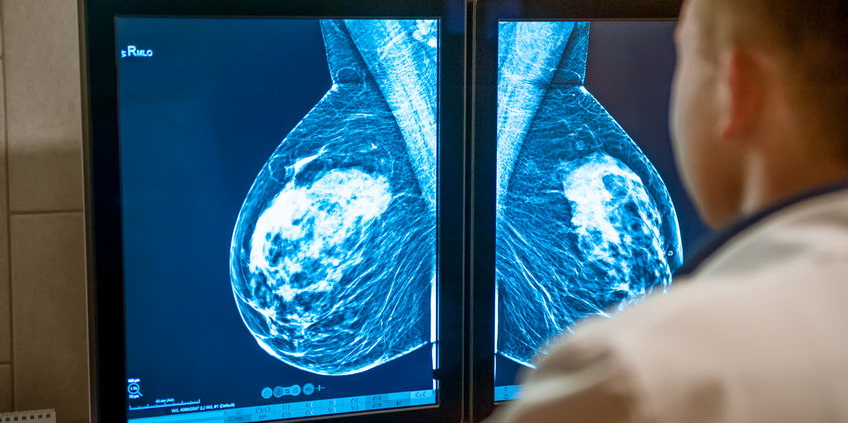
Approximately 60% of women undergoing annual screening mammography over a 10 year period will be called back for additional views. Often these are in women with dense breast tissue, which can make it more challenging to read mammograms. Many of these callbacks are false alarms, also known as false positives – the abnormality may resolve with additional views, it may be found to be a benign lesion (such as a fluid filled cyst), or a biopsy may be performed and the pathology is found to be benign.
In a study published in the journal Cancer Epidemiology, Biomarkers, and Prevention, researchers found that false positive mammograms are associated with an increased likelihood of eventually developing breast cancer. Using data from the Breast Cancer Surveillance Consortium, they noted that women who had a false positive mammogram with additional imaging or biopsy recommendation had a higher likelihood of developing breast cancer compared to women with a normal mammogram. For every 1,000 women who had a true negative mammogram, 3.9 developed breast cancer over a 10 year period (average follow up 5.4 years). For those requiring additional imaging, 5.5 / 1000 developed breast cancer over 10 years, and in those who underwent a biopsy 7 / 1000 eventually developed breast cancer. It is important to note that the absolute risk of developing a breast cancer in the case of a false positive mammogram was very low – less than 1%.
The group of women with the highest rate of breast cancer development were those with dense breast tissue who underwent a biopsy. This is not surprising, as we know that breast density increases the risk of breast cancer, and the number of prior breast biopsies is factored into risk assessment models such as the Gail and Tyrer-Cusik models.
At this point, it is not recommended that women who have a false positive mammogram undergo any specific additional imaging such as MRI (unless recommended based on the mammogram). A false positive mammogram is one risk factor, but it needs to be evaluated in the context of other breast cancer risk factors, such as increasing age, family history, obesity, and alcohol intake.
Additional Information:
Dr. Margaret Polaneczky blog post
Breast Screening Decisions – screening mammogram decision tool for women age 40-49
ASCO Post Commentary
NPR False Alarm Mammograms
HNR False Positive Mammograms and Cancer Risk