25 August 2016
A study published today in the New England Journal of Medicine reports on the 5 year results of the MINDACT (Microarray In Node-negative and 1 to 3 positive lymph node Disease may Avoid ChemoTherapy) trial. This study was designed to evaluate the use of a tumor gene signature test (MammaPrint) compared with standard factors to assess the need for chemotherapy.
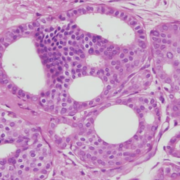
This study enrolled 6693 women in 112 countries who had undergone surgery for Stage I and II breast cancer. Once patients were registered, they were stratified based on risk. Risk was assessed both by the MammaPrint (MP) score as well as standard clinical – pathological markers (CP) such as tumor size, grade, ER/PR status, and Her2/neu expression calculated using the Adjuvant! Online tool.
2745 patients who had low risk MP and CP scores did not receive chemotherapy; 5 year metastasis-free survival in this group was approximately 97.6%. These findings were consistent with those reported using a different genomic test, the Oncotype Dx test, which also demonstrated good results without chemotherapy in low risk patients. 1806 patients who were high risk by both assessments received chemotherapy and 5 year metastasis-free survival in this group was approximately 90.6%.
The other 2 groups were those with discordant results, and these patients were randomized to either chemotherapy / endocrine therapy or endocrine therapy. The results for the 592 patients with high risk MP scores but low risk CP assessment are pending. The recently published study focuses on the 1550 patients with low risk MP scores but were high risk based on CP assessment.
The study demonstrated that in these patients, chemotherapy provided a slight benefit: 1.5% improvement in survival without metastatic disease, 1.4% improvement in overall survival, and 2.8% improvement in disease free survival. The study was not powered or designed to determine if these differences were statistically significant.
On the surface, the study seems to indicate that chemotherapy is of little to no benefit for those patients with low risk MP scores and high risk CP features. There is no question that genomic tests such as the MammaPrint have revolutionized our treatment recommendations. We now have the ability to obtain more detailed information about an individual patient’s tumor biology, which can help us guide treatment decisions. It is clear that our traditional methods of assigning risk such as tumor size, grade, and node status, do not always tell the whole story, and it is no longer acceptable to recommend chemotherapy “just to be sure”. The use of genomic tests in appropriate patients is very important to avoid the real dangers of over treatment. But as this study was not designed to assess statistical significance (rather, “non inferiority“), can we say that the benefits demonstrated from chemotherapy may not be important for an individual patient?
Median follow up in this study was was 5 years. 48% of patients were lymph node positive, 93% had grade 2 or 3 disease, and 34% were age 50 or younger. These factors are more often associated with an earlier risk of recurrence, so 5 years may be sufficient to note a difference in survival rates. It was also stated by the authors that “adjuvant chemotherapy exerts most of its beneficial effects early in the course of the disease”. However, they also noted that many of the tumors were ER+, which may recur well past 5 years. 10 year follow up is planned.
In an accompanying editorial, Drs. Hudis and Dickler point out that “although we may all agree that a 1% risk of distant metastasis at 5 years on the basis of genomic testing eliminates any potential benefit of chemotherapy, at what point would we begin to have differing opinions and perhaps mixed results from clinical trials? Answering this question is even more challenging, given that all chemotherapy is not the same in terms of efficacy or toxicity and that patients and health care providers bring subjectivity and personal values to their treatment decisions.”
As was pointed out during a recent online exchange (by a woman who had a low recurrence score and now has metastatic disease), these tests are not guarantees. While the numbers are low, some women in the low risk group developed metastatic disease. It is not known if chemotherapy would have been of benefit, but it does demonstrate how percentages are applicable to populations, not necessarily to individuals. We do not yet have a test that will predict the outcome with 100% certainty. The test results should be presented as part of a discussion which includes the patient’s preferences, values and concerns – concerns regarding cancer recurrence as well as potential side effects of therapy.