17 January 2016
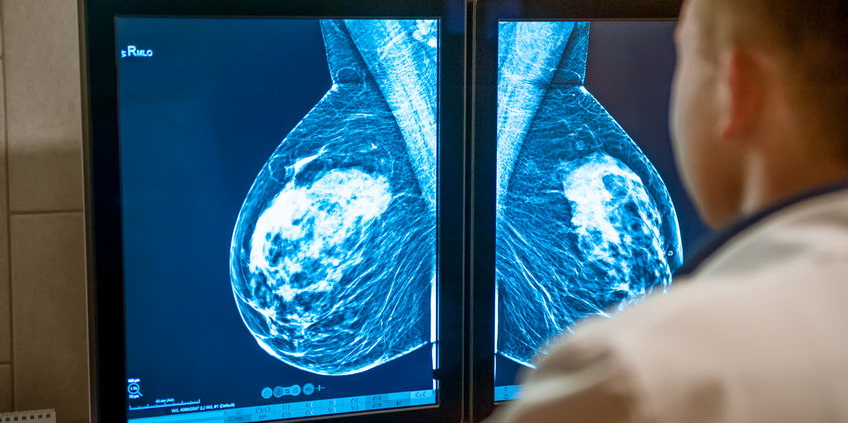
In October 2015, the American Cancer Society (ACS) updated their screening mammography guidelines, raising a lot of questions and concerns as annual mammograms were no longer recommended for all women starting at age 40. The United States Preventative Services Task Force (USPSTF) released new guidelines on screening mammography last week. The new USPSTF guidelines recommend an individualized risk-based approach for women age 40-49, and mammographic screening every other year for women age 50-74. The task force acknowledged that screening mammography reduces the likelihood of dying from breast cancer, but noted that the benefit was the greatest for women age 60-69, and the benefit was small for women age 40-49. For younger women, they noted that screening mammography is associated with higher false positives (false alarms).
The conflicting guidelines published by the USPSTF, ACS, and other organizations have caused much confusion. Many women simply want to know what they should do. The reality is, screening mammography is a one size fits all tool, and as any woman knows, that doesn’t really work. The sensitivity (“effectiveness”) of mammograms will vary depending on a patient’s age, menstrual status, use of hormone therapy, body mass index, breast density, and other factors. It is unrealistic to expect that one test can account for all of those variables, as well as personal risk factors for breast cancer, and personal preferences regarding screening risks and benefits.
To state it very simply:
- Mammograms may lead to improved survival from breast cancer by detecting some cancers early
- Some breast cancers are so aggressive that early detection does not lead to improved survival
- Mammograms are imperfect
It is important to note that the USPSTF and ACS recommendations apply to average risk women. Unfortunately, risk assessment is not routinely performed, and many factors associated with an increased risk, such as heavy alcohol intake and breast density, are not taken into account in the existing models. In an ideal world, we would swab a cheek, obtain some DNA, and then determine whether or not a woman is predisposed to develop breast cancer [I’m thinking beyond BRCA and other genetic testing here]. If we can determine that a 30 year old woman, even without a family of breast cancer, is predisposed to develop the disease, we can make educated screening recommendations (perhaps ultrasound and/or MRI, as mammograms are not very helpful in very young women). If we can determine that a woman is highly likely to die of a heart attack by age 60, and has no cancer predisposition, she might make the decision to forego screening mammography. Unfortunately we’re not quite there yet, but there are genetic risk tests under development.
I recently spoke with a researcher specializing in cancer risk. We discussed that at the end of the day, multiple organizations will continue to look at the evidence and draw different conclusions, so in his opinion, it wasn’t realistic that we should expect consensus. Physicians, researchers, and organizations are currently spending a lot of time and effort arguing with each other about whether mammography should start at age 40, if mammograms should be performed every versus every other year, and when screening should stop. However, our time and efforts might be better spent by working together to address issues such as disparities in access to screening mammography and lack of access to quality mammography and breast care for many women.
Recognizing the variability of each woman and her breasts, acknowledging the uncertainties regarding the risks and benefits of screening, and focusing on a shared decision making approach might help reduce some of the confusion. In medicine, as in many areas in life, there is often more than one right answer. The same applies to screening mammography. Time to move beyond the one size fits all approach.
Additional Reading:
New York Times: Panel Reasserts Mammogram Advice
JAMA: A Public Health Framework for Screening Mammography: Evidence-Based vs Politically Mandated Care
New York Times: Insurer Rewards Push Women Towards Mammograms
Forbes: A Turning Point in the Breast Cancer Screening Debate?
NPR Shots: Federal Panel Finalizes Mammogram Advice That Stirred Controversy
OncLive Final USPSTF Guidelines
Cornell Mammogram Decision Aid for Women age 40-49