7 April 2019
The Society of Surgical Oncology held their annual meeting in San Diego, CA from March 27-30, 2019. Approximately 1700 surgical oncologists were in attendance. As the organization is geared towards the entire field of surgical oncology, only a portion of the meeting covered breast cancer. Here are some of the highlights:
Genetic Testing and Management
Dr. Judy Garber – Dana Farber
Updates in Testing and Management of BRCA Mutations
– BRCA Mutation information from the National Cancer Institute
– Consider repeat testing if original genetic testing was performed prior to 2012 as more genes as well as pathogenic mutations have been discovered
– NCCN guidelines for breast cancer surveillance in BRCA 1/2 mutation carriers:
o Clinical breast exam every 6-12 months starting at age 25
o Annual MRI age 25-75 (individualize after age 75)
o Annual mammogram age 30-75 (individualize after age 75)
– NCCN guidelines for breast cancer prevention in BRCA 1/2 mutation carriers: discuss mastectomy, discuss tamoxifen
– Premenopausal BRCA mutation carriers who undergo oophorectomy experience breast cancer risk reduction. The level of breast cancer risk reduction in BRCA1 carriers is lower than in BRCA2 carriers as BRCA1-associated tumors are more likely to be triple negative
– Prenatal genetic testing is available in mutation carriers, and may be used for selective reproduction
– BRCA 1/2 mutation status does not impact breast cancer outcomes; tumor biology impact on outcomes is independent of mutation status
– BRCA 1/2 are DNA repair genes. Tumors associated with BRCA 1 tend to be triple negative and tumors associated with BRCA 2 tend to be ER/PR+, Her2- (but all combinations have been seen)
– Clinical trials are evaluating the use of cisplatin chemotherapy in patients with BRCA mutations – cancer cells are not able to repair DNA-induced chemotherapy damage due to the defective BRCA gene
– PARP inhibitors interfere with DNA repair and have traditionally been used to treat ovarian cancer. Small studies show some effect in breast cancer in the setting of BRCA mutations. Larger studies are ongoing. So far they only seem to work in breast cancer when there are BRCA mutations
– A challenge to treatment with PARP inhibitors is that there are many mechanisms of resistance, and tumors demonstrate a variable response to therapy – tests are being developed to predict response
– Lurbinectedin – a drug from sea slugs (!) may have some effect
– A very interesting comment – Dr. Garber noted that DNA breaks may be immunogenic, so there may be a role to combine PARP inhibitors and immunotherapy treatments
– Denosumab, a RANK-ligand used for bone protection in breast cancer patients, may have breast cancer risk-reducing activity – a randomized trial is pending to assess its activity as a preventative agent
Thuy Vu, Genetic Counselor – Wake Forest
What Genetic Test Should I Order?
– Once the appropriate patient for genetic testing has been identified, how to decide what lab to use? Consider lab experience, as well as cost and insurance support
– Patients with a complicated family history (multiple different cancers in scattered relatives), absent family history (adopted), and evidence of multiple cancer syndromes will benefit from NGS (next-generation sequencing) genetic panel testing
– A disadvantage of broad genetic panel testing is that there is currently incomplete information on all of the mutations that may be identified. Risk for cancers unrelated to the current diagnosis may be identified. In addition, there will be an increased prevalence of variants of uncertain significance (VUS)
– She noted to use caution when patients bring in test results from ancestry.com and similar companies – these sites often assess for SNPs (single nucleotide polymorphisms), which is not the same as testing for a genetic mutation, and full genetic testing may need to be repeated
– She acknowledged that there is a shortage of genetic counselors, even in large university centers. Many testing companies and labs now have associated genetic counselors, and there are some independent companies offering telephone counseling services
Dr. David Euhus – Johns Hopkins
ATM, CHEK2 and Other Genes
– While multiple gene mutations influencing breast cancer risk have been identified, they do not all convey the same level of risk
– As testing for multiple genes has increased, BRCA mutations are no longer the most common mutations found
– High risk genes include BRCA 1/2, TP53, PTEN, PALB2, STK11, CDH1
– Moderate risk genes include ATM, CHEK2, NBN, NF1
– These and other genes explain approximately 14-28% of genetic risk for breast cancer – most patients with a strong family history of breast cancer do not have an identifiable mutation
– There is a range of risk associated with all of the genes that in part depends on the mutation type – what type of damage does the mutation cause to the DNA. Family history of breast cancer can modify risk.
– For most of these patients, NCCN guidelines recommend annual MRI in addition to mammograms. Age to start supplemental screening depends on the mutation.
– He noted that increased screening for other associated cancers when there is no clinical benefit leads to patient harms – financial, emotional, and physical
– A good question from the floor about the role of ultrasound as supplemental screening (in addition to MRI) – Dr. Euhus states he uses 3D mammogram / tomosynthesis and does not use ultrasound unless the patient is pregnant / lactating
Dr. Kevin Hughes – Massachusetts General Hospital
What the Surgeon Needs to Know about Genetic Testing
– High cost of testing is not the problem – interpretation of the results is the challenge
– Assuming that approximately 10% of breast cancers are hereditary, over 51,000 breast cancers could have been prevented with testing
– For the breast surgeon, understanding BRCA 1/2 is not enough. There are many genes, each have different spectrum of associated cancers and associated risk; treatment needs to be individualized for the patient taking into account their specific mutation and family history
– He emphasized the point Dr. Garber made that if testing on a breast cancer survivor was performed prior to 2012, those patients should be re-tested
– Recent American Society of Breast Surgeons guidelines call for consideration of genetic testing in all breast cancer patients
– Dr. Hughes notes that this is already a standard recommendation for other cancers such as ovarian, pancreas and others
– The field is becoming more complicated – it is not expected that anyone can memorize this – go to the internet and look it up!
Resources:
ASK2ME – All Syndromes Known to Man Evaluator
ClinVar – look up specific mutations to see how they have been classified
PROMPT registry for patients with rare mutations
Breast Cancer Treatments in the Young and Elderly
Dr. Mina Sedrak – City of Hope
Treatment Strategies in Octogenarians with Early Stage, High-Risk Breast Cancer
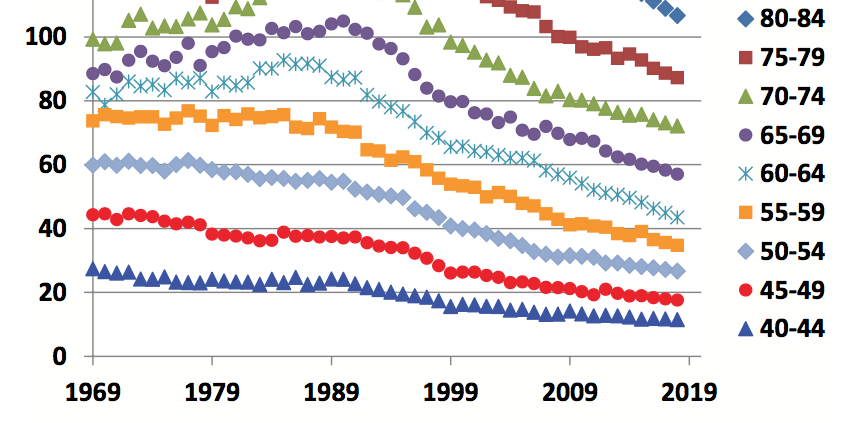
– Incidence and mortality from breast cancer increase with age; the number of older adults in the US is increasing
– Breast cancer outcomes are often worse for older (as well as younger) women
– Older adults are underrepresented in cancer clinical trials – 1/3 of patients with breast cancer are over the age of 70, but only a small percentage of them are included in clinical trials
– Because of lack of clinical trial data in older women, patients may be under- or over-treated [DJA note – we have a similar situation in men with breast cancer].
– There is no universal definition of “old”. Aging is a continuous spectrum, and chronological age does not accurately predict functional age. The ASCO Guidelines Geriatric Assessment can help understand factors other than chronological age to predict morbidity and mortality. US Life Tables can also be used to estimate life expectancy, as well as ePrognosis. Estimation of life expectancy should be performed for all older patients before making a treatment plan
– How to best treat cancer in the elderly patient: it depends on life expectancy, aging concerns, risks / benefits of treatment and the potential impact of co-existing medical problems
– What risks can we modify and what are the patient preferences? There is no “one size fits all”
Dr. Tyler Chesney – University of Toronto
Adjuvant Radiotherapy for Older Women after Breast Conserving Surgery
– 4 randomized clinical trials addressed if elderly patients with low-risk breast cancer need radiation therapy after breast conserving therapy: NSABP B-21, A. Fyles, CALGB 9343, and PRIME II studies
o Meta-analysis of these 4 studies: 2387 patients across all trials, early stage breast cancer, hormone receptor positive. Addition of radiation therapy reduces local recurrence from 60 versus 10 / 1000 at 5 years. 2 trials had 10 year follow up, noting recurrence was 80 versus 20 / 1000 women.
o 3 of the trials provided data on axillary recurrence: absolute benefit was small, 12 versus 3 / 1000 women. No difference in distant recurrence or overall survival
– Prime I study showed that older women who underwent radiation therapy had increased fatigue over 5-10 years but similar overall health-related quality of life
– Accelerated partial breast irradiation may be an option, but some studies have shown higher local recurrence and poorer cosmetic result (depending on treatment method)
– While toxicities of radiation therapy have improved with more modern techniques, logistical concerns such as time, need to travel, and cost may be of higher concern for older women
Dr. Laura Dominici – Dana Farber Cancer Institute
Reconstruction and Body Image in Young Patients
– More than 13,000 women under the age of 40 are diagnosed with breast cancer annually in the US, approximately 7% of all new diagnoses
– Younger women newly diagnosed with breast cancer have been shown to have higher rates of anxiety and distress after diagnosis, they have historically received more aggressive treatment, and have a long survivorship period
– More aggressive surgery such as mastectomy does not lead to improved overall or breast cancer specific survival. Local recurrence is related to tumor biology, not age of the patient
– Mastectomy (single and bilateral) rates are rising, especially among younger women. Rates of reconstruction are increasing, as are rates of post mastectomy radiation
– A growing number of patients are “going flat” after mastectomy, opting for no reconstruction
– Dana Farber young women’s multicenter prospective cohort study: poorer satisfaction with breast-related, psychosocial and sexual well-being after unilateral and bilateral mastectomy. Other factors impacting poorer satisfaction include financial status, lymphedema, and the need for radiation
– 42% of women age 50 and younger (in the Dana Farber study) regret their surgical decision including primary surgery and reconstruction decision. Patients in this study were not asked what the actual regret was – doing too much or too little
– Important for patients to understand the oncologic outcomes of their decisions, and for physicians to promote shared decision making that takes into account patient preferences and concerns
Dr. Jo Chien – University of California, San Francisco
Fertility in Young Breast Cancer Patients
– 51% of women under age 40 with breast cancer are concerned about fertility; 38% desire to have future children but up to 97% are at risk of treatment related infertility. 26% report that their concerns about infertility affected their treatment decisions
– Loss of reproductive potential after cancer treatment results in worse long-term quality of life, unresolved grief / depression, reduced life satisfaction. Fertility preservation associated with less regret among young cancer survivors
– Less than 25% of general oncologists refer young breast cancer patients to fertility specialists
– Factors impacting risk of chemotherapy-induced ovarian failure: older age, baseline ovarian reserve, type of chemotherapy, and chemotherapy dose / duration
– Menses is not a surrogate marker for fertility. Fertility decline occurs ~10 years before onset of menopause. For women who remain premenopausal after chemotherapy, the majority enter menopause prematurely
– Options for fertility preservation: ovarian stimulation and cryopreservation of embryos / oocytes, GnRH agonists, and experimental techniques such as cryopreservation of ovarian tissue and immature oocyte retrieval with in vitro maturation
– Several studies have evaluated safety of letrozole-gonadotropin protocol in women with breast cancer and have found no difference in relapse-free survival. Very limited data on safety of ovarian stimulation in the neoadjuvant setting. In subset (82 patients – 34 stimulation / 48 controls) of I-SPY2 trial, no delay in start of neoadjuvant treatment and no significant difference in pCR or recurrence or mortality rates in patients who underwent ovarian stimulation before chemotherapy
– As discussed in the genetics session, Dr. Chien noted that for BRCA mutation carriers, pre-implantation genetic diagnosis is an option. Multiple follicles / embryos are required, often needing multiple stimulation cycles
– Observational studies suggest that pregnancy is safe after breast cancer.
– When is it safe to become pregnant after treatment? It comes down to patient’s underlying risk and likely their risk aversion. Dr. Chien prefers to wait to 2-3 years, but notes there is no data to support that. The POSITIVE trial is studying the impact of adjuvant endocrine therapy interruption to allow for pregnancy
Key papers
Dr. Kandace McGuire from Virginia Commonwealth University Massey Cancer Center provided an overview of 3 practice-changing papers from 2018. She noted at the start of her talk that while this is a surgical audience, all of the studies were from the medial oncology literature. This comment highlighted the multidisciplinary nature of breast cancer care – the entire treatment team needs to be aware of the latest advances and updates.
The TAILORx study assessed Oncotype Dx results and noted that many patients previously classified as intermediate risk could now be classified as low risk. Therefore, a larger percentage of patients do not need chemotherapy. However, questions remain for patients under the age of 50.
The TEXT / SOFT trials evaluated the use of ovarian suppression in premenopausal women with hormone receptor positive breast cancer. Ovarian suppression resulted in improved disease free and overall survival, but the magnitude of improvement varied according to recurrence risk. High risk patients may have 10-15% improvement. However, quality of life and fertility may be impacted by ovarian suppression in these younger women
The KATHERINE study assessed the use of TDM1 in patients with Her2/neu over-expressed tumors who did not exhibit a pathologic complete response (pCR) after neoadjuvant (before surgery) chemotherapy. Those who received adjuvant TDM1 versus trastuzumab showed an improved disease free survival, but more study is needed to assess the effect on overall survival.
Dr. V. Craig Jordan delivered the American Cancer Society / SSO Basic Science Lecture: The SERM Saga: Something From Nothing. Dr. Jordan’s presentation was a nice history lesson about the discovery and use of tamoxifen as a treatment for breast cancer.
– Dr. Jordan noted the early clues that endocrine therapy might be effective for some breast cancers – removal of the ovaries, adrenal glands, and even part of the pituitary gland led to improved outcomes (with a fair amount of associated risk)
– Tamoxifen was initially developed as a contraceptive agent, but it was not successful and was going to be discarded by the manufacturer
– The link to endometrial cancer and tamoxifen was initially denied, despite some interesting studies by Dr. Jordon noting the association. He noted that the early studies evaluating tamoxifen simply did not assess for endometrial cancer
– He noted that the cumulative frequency of uterine cancer with 2 years of tamoxifen is ~1.5%, and with 5 years of tamoxifen ~5.5%. He commented that if the studies were performed today, the data monitoring committees would “go apoplectic” over these results
– Raloxifene in early studies showed decrease in breast cancer but also decrease in bone fractures – this led to the STAR trial which assessed the ability of raloxifene and tamoxifen to reduce breast cancer development in high-risk women
– He discussed other drugs, derived from tamoxifen, that are being developed – searching for those with improved side effect profiles
– He quoted George S. Patton: “If everyone is thinking alike, then someone isn’t thinking”
Presidential Address – Serendipity and Strategy on the Path of Progress
Dr. Armando Giuliano, known to some as the “father” of the sentinel node biopsy, provided some interesting details on how his research process unfolded. He noted that “my success has been due to good luck, mixed with hard work, strategic planning, and serendipity.” Like those before him who proposed less aggressive surgical therapy for breast cancer, he was met with a fair amount of criticism. Patients and surgeons have benefited from his perseverance and dedication.
All of the research abstracts and posters can be found here. There were many interesting and thought-providing presentations, but it is important to remember that abstracts have not been subject to the peer-review process, and may represent incomplete data.
As usual if anyone is interested in one of the articles but does not have access, please send your email address to me: contact at drattai dot com and I will be happy to send you a copy.
This post has not been endorsed by the Society of Surgical Oncology.