12 December 2019
A study presented at the San Antonio Breast Cancer Symposium last week provides more evidence to support the use of accelerated partial breast irradiation (APBI) after lumpectomy in selected patients with breast cancer.
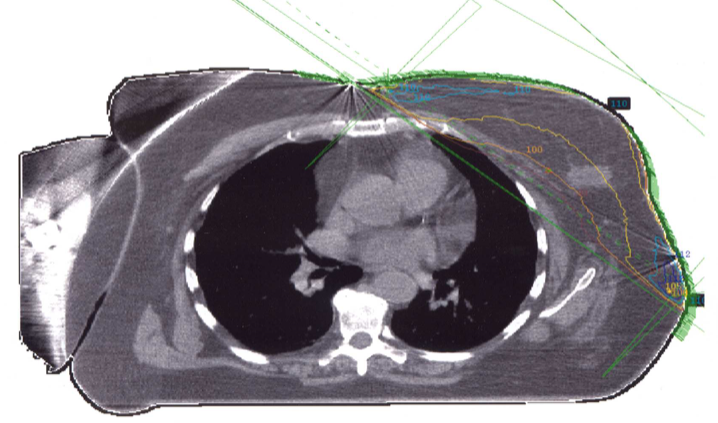
Radiation after lumpectomy typically treats the entire breast (whole breast irradiation, WBI) and is usually administered daily for 3-6 weeks, depending on the protocol that is used. There are several techniques that treat only the lumpectomy site, which is where most recurrences occur. The techniques include the use of a single or multiple catheters, or an external beam approach. Most commonly, partial breast treatment is administered twice a day for 5 days. Of course, one of the concerns in using a partial breast technique is recurrence rates compared to the more standard WBI approach.
A large US-based study on partial breast irradiation was presented in 2018 and was recently published. The NSABP B-39 trial* included 4200 patients, randomized to WBI or APBI techniques. This study showed that APBI was “not equivalent” to whole breast irradiation but absolute differences in local recurrence rates were small (90 / 4% in the APBI group versus 71 / 3% in the WBI group).
The current study (APBI IMRT Florence) was performed in Italy and included 540 patients. All were over age 40, had tumors ≤ 25mm in size, and surgical margins ≥5mm [note – current US national guidelines support “no ink on tumor” for a margin]. The findings included:
- Local (in-breast) recurrence rates were 3.9% (9 patients) with APBI and 2.6% (6 patients) with whole breast irradiation and that difference was not statistically significant
- Overall survival was 92.7% in the APBI group and 93.3% in the WBI group
- Breast cancer-specific survival was 97.6% in the APBI group and 95.7% in the WBI group
- There were 7 patients in each group who developed metastatic breast cancer
- There were fewer adverse events and better cosmetic results reported in the APBI group compared to the WBI group
The authors concluded that APBI is appropriate to consider in selected patients with “low risk” cancers. While the Italian study has only been presented in abstract form (we do not have the full dataset or manuscript yet), it adds to what we already know about this accelerated technique, which does seem to be a reasonable option in selected patients.
*If you are not able to access the full study and would like a copy, please email me: contact at drattai dot com