12 September 2017
A common misconception among patients is that more aggressive surgery for breast cancer leads to better outcomes. In fact, nothing could be further from the truth. The standard operation for breast cancer for years (up until the 1960-70s) was the Halsted radical mastectomy, during which the breast, pectoralis muscle of the chest, and underarm lymph nodes were all removed. Randomized trials then showed that less aggressive surgery, including lumpectomy, resulted in similar survival rates as the more extensive procedure. Axillary lymph node dissection, or removal of a large number of underarm lymph nodes, was also a standard procedure for any patient with breast cancer. Studies performed in the late 1980s reported on the accuracy of the sentinel node biopsy technique, which involves removal of only a few targeted underarm lymph nodes. Adoption of that procedure resulted in decreased rates of arm swelling (lymphedema) and did not negatively impact recurrence or survival rates.
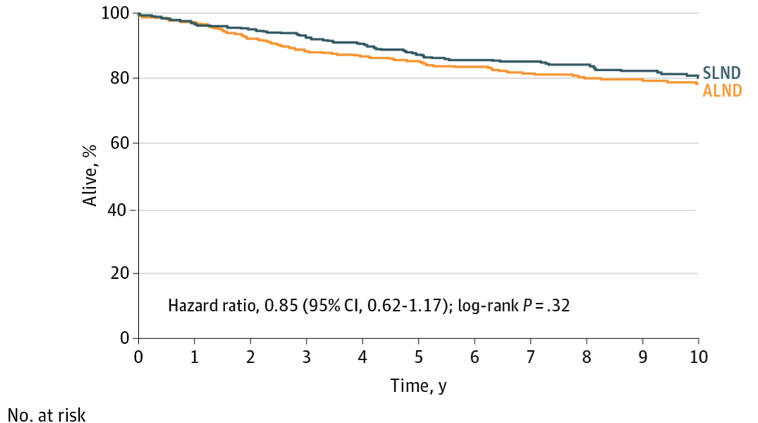
Up until about 10 years ago, it was standard practice to test the sentinel nodes in the operating room and if cancer cells were found, complete axillary dissection would be performed. Published in 2011, the American College of Surgeons Oncology Group Z11 study showed that the addition of axillary dissection did not impact local recurrence (cancer coming back in the underarm) or survival rates. This changed practice immediately – and many more women were spared from undergoing full lymph node removal. The 10 year follow up results to Z11 were just published, and confirm the earlier studies noting similar disease-free and overall survival in patients undergoing sentinel node biopsy alone.
It is important to note that the “Z11 criteria” do not include all patients. Women in the study had early stage breast cancers, were “clinically node negative” (not able to feel any underarm lymph nodes), and only had 1 or 2 involved sentinel nodes. All patients in the study had lumpectomy, followed by chemotherapy and radiation. Patients with more than 2 involved lymph nodes, patients who are being treated by mastectomy, or those who receive chemotherapy or hormonal therapy prior to surgery still may need to undergo the more extensive axillary node dissection. Studies are ongoing to see if we can minimize surgical therapy in these patient populations, because over the years, we have found that more aggressive surgery only leads to more complications, not better outcomes.
Additional Information:
The Atlantic – How Clinical Trials Saved Women With Breast Cancer From Disfiguring Surgery (2013)