14 October 2015
The discussion on whether or not DCIS is cancer, and how best to treat it, continues.
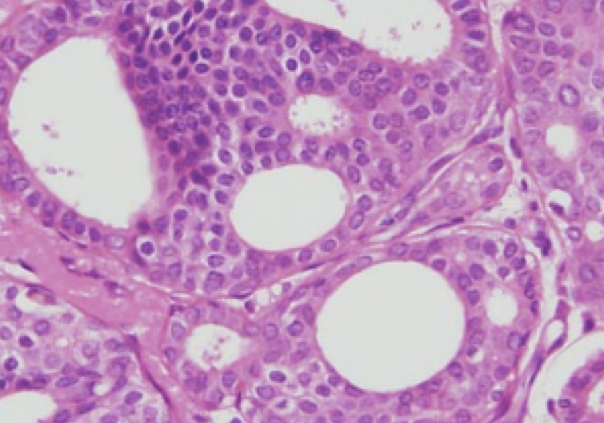
A study published recently in the Journal of Clinical Oncology by Dr. Lawrence Solin and colleagues evaluated the risk of developing an invasive cancer if radiation therapy was not performed after lumpectomy for DCIS. This was a prospective non-randomized trial. Patients were enrolled from 1997 – 2002. Patients were divided into 2 groups: 1.) low or intermediate grade DCIS, tumor size 2.5cm or smaller (561 patients), and 2.) high-grade DCIS, tumor size 1cm or smaller (104 patients). All patients underwent lumpectomy but none received radiation therapy.
The study reports 12 year results. There were 99 “in-breast events” (IBE – a new DCIS or invasive cancer), 51 (52%) were invasive. The rates of all IBE and invasive IBE continued to increase during the surveillance period. The 12 year rates of developing an IBE were 14.4% for the low-risk group and 24.6% for the high-risk group. The 12 year rates of developing an invasive IBE were 7.5% for the low-risk group and 14.3% for the high-risk group. In addition to low or high-risk category, tumor size was correlated with risk of recurrence. Patient age, menopausal status, size of surgical margin, use of tamoxifen, or prior use of hormone replacement therapy were not associated with risk of developing an IBE.
The authors concluded that “individual patients and their physicians will need to decide if these 12-year risks are acceptable, and to judge whether or not to add adjuvant treatment [radiation and/or hormonal therapy such as tamoxifen] after surgical excision. Not all patients and their physicians will agree on what is considered too high a risk of developing an IBE or an invasive IBE to recommend observation after surgical excision, or what risk is considered too low to justify adding radiation treatment.” While this may lead to more confusion on the part of patients, it points out the need for careful discussion of the risks and benefits of treatment and observation, as well as an assessment of an individual’s risk tolerance.
Adding to the DCIS discussion, was an abstract presented at the 2015 American Society of Clinical Oncology Breast Cancer Symposium. Dr. Kimberly VanZee and colleagues presented an abstract on recurrence rates of DCIS. They retrospectively reviewed a database of DCIS cases between 1978 – 2010 at the Memorial Sloan Kettering Cancer Center in New York. There were 363 (12%) recurrences in 2996 cases. The 5-year recurrence rate from 1978 – 1998 was 13.6% versus 6.6% between 1999 – 2010. Interestingly, the decrease in recurrence rates were limited to patients who did not undergo postoperative radiation therapy. There was no decline in recurrence rates during the 2 time periods in patients who received radiation therapy. They concluded that the rates of recurrence after treatment for DCIS are declining over time, possibly due to improvements in detection and pathologic assessment. The authors felt that it was important to stress to women with DCIS that are considering mastectomy, that while recurrence is a possibility after treatment for DCIS, the rates are very low. This was presented as an abstract and not a full manuscript – I am looking forward to more detailed analysis and discussion when the full paper is published.
The Breast Cancer Symposium also featured a pro-con debate between Dr. Ben Smith (radiation oncologist from MD Anderson) and Dr. Shelley Hwang (surgical oncologist from Duke University). The topic – “Is DCIS Cancer?”. Dr. Smith took the pro / yes position, and Dr. Hwang took the con / no position. Both gave excellent presentations, citing compelling studies and statistics. They both gave a similar analogy, presenting progression of DCIS to invasive cancer as a “crime”. Dr. Smith took the position of wanting to stop the crime before it happened:
B Smith fun analogy in DCIS: Is it cancer? debate at #bcs15 when would you intervene? pic.twitter.com/WkCBQIjYdD
— Julie Gralow (@jrgralow) September 26, 2015
While Dr. Hwang noted “should everyone be punished as if they would commit a crime?”
Love this rebuttal slide from Dr. Hwang @DukeCancer Which of these kids is ‘the problem’? #bcs15 #bcsm pic.twitter.com/qxfnq1RT6K — IBC Research Fdn (@IBCResearch) September 26, 2015
It was definitely an entertaining and spirited debate, but unfortunately we still don’t have the answers for an individual patient faced with this diagnosis.
This isn’t just a discussion that breast cancer specialists are having. A TIME Magazine story: Why Doctors are Re-Thinking Breast Cancer Treatment also addressed the concerns about over-diagnosis and over-treatment, especially for low-grade DCIS. I think the story did a good job covering the controversy over screening mammograms and it raised some good points about cancer treatment and medical progress. It’s worth a read.
NPR discussed a study recently published in the Journal of the National Cancer Institute – Trends in Treatment Patterns and Outcomes for Ductal Carcinoma In-Situ. This was a study using the SEER Registry. 128,080 patients treated for DCIS between 1991-2010. They found that over time, the number of women treated by lumpectomy and radiation increased, while the number of women treated by mastectomy decreased. However, there was an increase in the rate of bilateral mastectomy for DCIS – 0% in 1991 and 8.5% in 2010. The rate of women opting for no treatment increased from 1% to 3% during the study period.
Overall survival was 89.6% in women who underwent lumpectomy and radiation, 86% for those who underwent mastectomy, and 80% for those who underwent a lumpectomy without radiation. However, only 9% of overall deaths were due to breast cancer – the majority of deaths were due to cardiovascular disease. It is well known that more women in this country die due to cardiovascular disease than from breast cancer. Deaths specifically from breast cancer (more relevant than overall survival) were identical for the lumpectomy-radiation, mastectomy, and lumpectomy alone groups. This again raises the need for additional research into which women will truly benefit from treatment for DCIS.
And finally (for now, anyway), Dr. Laura Esserman and others were quoted in an ASCO Post article: Where We Have Been and Where We Can Be. The authors elaborated on points that were made in an August 2015 JAMA Oncology editorial: Re-Thinking the Standard for Ductal Carcinoma In-Situ Treatment. The authors suggested that radiation therapy not be routinely recommended after lumpectomy when the DCIS is not high-grade, as there has been no demonstrated survival advantage. They also suggested that low- and intermediate-grade DCIS should not be a target of screening and early detection. They noted significant challenges in abandoning the use of radiation and decreasing the number of biopsies performed for calcifications that likely represent low grade disease. They also called for more research to be performed to understand the biology of the highest-risk lesions and patient populations.
To be continued…



Trackbacks & Pingbacks
[…] Influential People – Laura Esserman and Shelley Hwang Dr. Attai Active Surveillance for DCIS Dr. Attai DCIS Continued… Dr. Attai slideshare Are We Overtreating DCIS? DCIS411 Health News Review Podcast – Active […]
[…] Information: DCISOptions.org DCIS, Continued… CBS News: Dr. Laura Esserman – When is it OK Not to Treat Cancer? HealthNews Review Podcast: […]
Comments are closed.